How Britain Creates Mental Illness: Racial Inequity, Misdiagnosis and a System that Won’t Change
Racial equity in mental health requires more than a yearly regurgitation of the same tired statistics. In 2025, we don’t need more evidence, we need the integrity to act on what we have.

Note: These problems are not unique to the UK. Across Western nations, Black populations face similar issues.
Society’s tendency to blame the victim has always made me indignant, especially the pathologization of ethnic minorities. In the early 2000s, I became aware of the high rates of severe mental illness among Black people in the UK, often framed as individual pathology. This prompted me to research the issue, leading to a 2008 article, Racializing Mental Illness.
“I argued for a shift in focus. Instead of asking what is ‘wrong’ with individuals, we must consider their societal experiences.”
In the article, I discussed how negative racialized experiences likely contribute to the higher schizophrenia rates among Black individuals in the UK (6 to 18 times higher than White Britons). I argued for a shift in focus. Instead of asking what is “wrong” with individuals, we must consider their societal experiences. Factors such as minority status stress, stress linked to racial discrimination and racial bias in psychiatric diagnosis are potential causes of these high schizophrenia rates.
To illustrate minority status stress, I called attention to findings showing that ethnic minorities have higher rates of schizophrenia in places where they make up a smaller percentage of the population. Lone minority individuals lack the psychological safety of a larger ethnic group, leaving them vulnerable to isolation and marginalization. In this context, it shouldn’t be surprising that Black individuals in the UK — who represent a tiny proportion (3.7%) of the overall population — are more susceptible to mental health issues.
“Lone minority individuals lack the psychological safety of a larger ethnic group.”
To explain the reality of racism-induced stress, I cited research linking racial discrimination to a higher risk of psychotic disorders. Indeed, discrimination affects mental health through microaggressions (everyday acts of subtle racial aggression); harassment (e.g., slurs, physical attacks); and systemic inequities (e.g., in employment, healthcare, education, criminal justice). These relentless stressors can wear down even the strongest individuals. Thus, this isn’t rocket science; it is reasonable to draw the conclusion that this level of social adversity can indeed lead to mental illness among marginalized minorities.
I also suggested that racial bias in psychiatric diagnosis might help explain the persistently high schizophrenia rates among Black Britons. Psychiatrists often over diagnose schizophrenia while under diagnosing conditions such as depression in Black patients. Even today, reliance on Western diagnostic tools leads psychiatrists to mislabel protective behaviours such as “healthy cultural paranoia,” as severe mental illness.
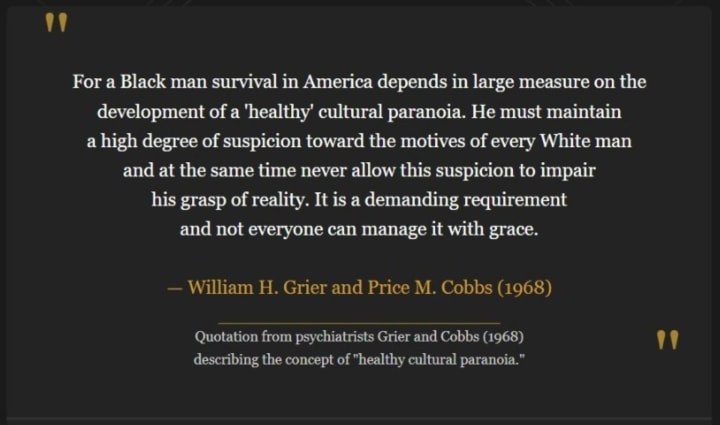
Research also shows significant differences in diagnoses between Black and White psychiatrists, supporting the theory that racial bias contributes to these high schizophrenia figures in Western countries.
What’s changed since 2008?
Since 2008, awareness of the social determinants of mental health has grown, with discussions linking discrimination to mental illness becoming less taboo, though still controversial. However, this increased awareness hasn’t resulted in meaningful changes. The persistent impact of systemic discrimination on mental health and continued inequities in mental health services is illustrated by recent reports:
- A 2019 comprehensive review of research shows that Black Africans and Caribbeans are still 5–6 times more likely to be diagnosed with schizophrenia as compared with the White population in England.
- Black people remain 3.5 times as likely as White people to be detained under the Mental Health Act (2023 government data).
- The persistence of racial bias in mental health services is evident in the findings of a 2024 University College London study. Researchers found that Black patients with severe mental illness in the UK are given higher doses of antipsychotics than their White counterparts, exposing them to a greater danger of side effects.
- A 2024 report by mental health charity Mind, which operates in England and Wales, reiterates what’s been known for decades: Black people are more likely to be diagnosed with psychosis; less likely to be offered psychotherapy; and more likely to face heavy-handed treatment, including detention under the Mental Health Act, forced medication, and confinement in isolation rooms.
A 2025 Call to Action
Seventeen years after publishing my 2008 article, cultural incompetence in UK mental health services remains as entrenched as ever. Despite an increased recognition of social determinants of mental health (particularly among scholars and policy experts) this knowledge isn’t being translated into meaningful progress. Even after the global racial reckoning of 2020, academic and policy literature on racial inequities continues to be recycled every year, without any promise of systemic reforms. So, in 2025, this is another call to action:
- Mandate equity-focused diagnostic tools that avoid pathologizing Black distress.
- Legally require that racial trauma-informed therapy - acknowledging the social realities of Black individuals - is standard practice.
- Legislate training in equity-focused diagnostic tools and racial trauma-informed therapy in mental health education curricula (psychiatry, psychology, counselling).
- Promote ethnic patient-clinician matching to enhance empathy and understanding of race-related stressors.
- Develop and commit to a strategy that expands the recruitment and retention of Black mental health professionals.
Racial equity in mental health requires more than a yearly regurgitation of the same tired statistics. In 2025, we don’t need more evidence, we need the integrity to act on what we have.
The 2008 paper referred to in this article can be viewed here.
[A version of this article was originally published by the Medium publication "An Injustice!" on May 21, 2025.]
About the Creator
Clare Xanthos
Researcher & Writer. Interests: racial equity, social justice, cultural identity. Co-editor & an author of 2 chapters in the book "Social Determinants of Health among African-American Men." PhD in Social Policy (London School of Economics).






Comments
There are no comments for this story
Be the first to respond and start the conversation.