Latest Stories
Most recently published stories in Longevity.
FridaBaby Faces Backlash Over Alleged Sexualized Marketing of Infant Products
The baby-care brand FridaBaby, known for products such as the NoseFrida nasal aspirator and infant thermometers, is facing a surge of online backlash following the resurfacing of old marketing materials featuring suggestive and sexualized language. Social media users have widely circulated screenshots of posts and product packaging, criticizing the brand for content deemed inappropriate for items designed for infants.
By Story Prism20 days ago in Longevity
James Van Der Beek’s Colon Cancer: A Warning for Young Adults
The sudden news of James Van Der Beek’s death at 48 shocked fans worldwide, not just because of the loss of a beloved actor, but also because it highlights a growing public health concern: colorectal cancer in younger adults. Best known for his roles in Dawson’s Creek and Varsity Blues, Van Der Beek’s journey with stage-3 colorectal cancer underscores the importance of recognizing subtle symptoms, seeking early medical evaluation, and understanding that cancer is not limited to older adults.
By Story Prism20 days ago in Longevity
Rise in Half-Term Holiday Bookings After Rainy January. AI-Generated.
A surge in half-term holiday bookings has been reported across the UK following one of the wettest and dullest Januarys in recent years, as families seek sunshine and a change of scenery after weeks of persistent rain and cold weather. Travel companies say demand for February half-term trips has increased sharply, with popular destinations including Spain, the Canary Islands, Turkey, and parts of the Middle East. Domestic breaks have also seen a boost, particularly in countryside and coastal areas, as people look to escape the gloomy conditions experienced at the start of the year. According to forecasters at the Met Office, much of the UK experienced above-average rainfall and limited sunshine throughout January, contributing to low public morale and a strong desire for travel. “After such a grey and wet start to the year, many families are looking for a mental and physical reset,” said one senior travel industry executive. “Half-term offers the perfect opportunity to get away, and bookings reflect that mood.” Families Lead the Travel Boom Tour operators report that families with school-aged children are driving the increase in demand. With limited travel opportunities during term time, half-term remains one of the busiest periods of the year for leisure travel. Beach destinations are proving especially popular, with resorts in southern Europe and North Africa offering warmer temperatures and family-friendly packages. Ski resorts in France, Austria, and Switzerland have also seen higher booking levels, helped by improved snow conditions following an inconsistent start to the winter season. One London-based parent said the decision to book a holiday was spontaneous. “We were stuck indoors for weeks because of the rain. As soon as half-term came up, we decided we needed a break somewhere bright and warm.” Industry Sees Economic Lift The travel sector has welcomed the uptick in bookings as a sign of renewed consumer confidence after a difficult period marked by high living costs and inflation. The Association of British Travel Agents (ABTA) said the pattern suggests that households are prioritizing experiences despite financial pressures. “Even with tight budgets, families still want something to look forward to,” an ABTA spokesperson said. “We’re seeing people booking shorter trips or choosing budget-friendly destinations, but they are booking in large numbers.” Travel analysts say the rainy January created a psychological push toward travel, with many consumers reacting emotionally rather than purely financially. Social media trends showing sunny beaches and winter sun deals also contributed to the sudden spike in interest. Domestic Tourism Benefits Too It is not only overseas holidays seeing growth. UK holiday parks, countryside cottages, and spa hotels have reported increased reservations for half-term week. Businesses in regions such as Cornwall, the Lake District, and parts of Wales say families are opting for short domestic breaks rather than longer foreign trips, partly due to convenience and cost. A hotel owner in Devon said enquiries doubled compared with the same period last year. “People just want to get out of their homes and enjoy some fresh air. Even if the weather is still cool, a change of environment makes a big difference.” Weather’s Powerful Influence Experts note that weather plays a major role in travel decisions, particularly during winter months when people are more sensitive to prolonged cold and rain. Psychologists say gloomy weather can affect mood and motivation, increasing the desire for sunshine and outdoor activities. January’s persistent rain and limited daylight may have intensified that effect this year. Some airlines have added extra capacity on popular routes, while budget carriers have reported fuller flights than expected for the February period. Travel websites have also recorded higher search volumes for destinations associated with warmth and sunshine, suggesting that “winter escape” travel has become more emotionally driven. Cost and Accessibility Despite rising interest, cost remains a key factor. Many families are booking earlier in order to secure discounts, while others are opting for shorter stays or off-peak flights. Package holidays continue to dominate, as they offer fixed prices and reduce uncertainty around accommodation and transport costs. Travel agents say there has been increased interest in all-inclusive resorts, where families can manage spending more easily without worrying about daily expenses. Looking Ahead Industry experts believe the trend could continue into the Easter holidays if weather conditions remain unsettled in the UK. However, they caution that sustained demand will depend on economic stability and consumer confidence. For now, the post-January travel surge reflects a broader desire to reclaim leisure time after a long and difficult winter start. “People feel they deserve a break,” said one travel consultant. “After weeks of rain, the idea of sunshine or even just a different place has become incredibly appealing.” As half-term approaches, airports and tourist destinations are preparing for a busy period, while families across the country count down the days to a well-earned escape from the lingering winter blues.
By Fiaz Ahmed 20 days ago in Longevity
China’s Yangtze River Shows Signs of Remarkable Recovery After Fishing Ban. AI-Generated.
The mighty Yangtze River, long strained by pollution, overfishing, and heavy industrial use, is showing clear signs of ecological recovery following the government’s landmark 10-year fishing ban. Scientists and environmental officials report rising fish populations, improved water quality, and the return of species that had nearly vanished from large stretches of the river. The fishing ban, introduced in 2021, covers more than 300 tributaries and lakes connected to the Yangtze and affects hundreds of thousands of fishermen. It was one of the most ambitious conservation policies China has ever implemented for a single river system. The Yangtze basin supports nearly one-third of the country’s population and contributes significantly to agriculture, shipping, and hydropower, making its health crucial for both people and nature. Recent monitoring data released by China’s environmental authorities show encouraging results. Surveys conducted across multiple provinces found that the number of native fish species has increased steadily since the ban began. In some areas, biodiversity has risen by more than 20 percent compared with levels recorded before 2020. Aquatic plants have also begun to regenerate along riverbanks, helping stabilize soil and provide shelter for fish and birds. One of the most significant developments has been the partial return of rare species once pushed to the brink by decades of overfishing and dam construction. Although the Yangtze river dolphin, or baiji, is considered functionally extinct, conservationists have reported increased sightings of the Yangtze finless porpoise, another endangered species that depends on healthy fish stocks. Experts say the porpoise’s improved survival rates are a strong indicator that the ecosystem is slowly repairing itself. Water quality has also shown measurable improvement. Government testing stations along the river report lower concentrations of ammonia nitrogen and other pollutants linked to industrial waste and agricultural runoff. While pollution remains a challenge in heavily urbanized sections, the overall trend suggests that reduced fishing pressure has helped restore balance between species and improved natural self-cleansing processes within the river. Officials from the Ministry of Agriculture and Rural Affairs say enforcement of the ban has strengthened in recent years, with patrols using drones and satellite tracking to prevent illegal fishing. Thousands of boats have been removed from service, and penalties for violations have increased. Local governments have also expanded protected zones and wetland parks along key stretches of the river. The human impact of the ban has been significant. More than 230,000 fishermen were forced to give up their livelihoods, prompting concerns about unemployment and social stability. In response, authorities launched retraining programs to help former fishermen find work in tourism, environmental monitoring, and aquaculture outside protected zones. Some communities have developed river-based eco-tourism projects, offering boat tours and wildlife viewing experiences that depend on a healthy ecosystem. In cities such as Wuhan, residents have noticed visible changes. Locals report seeing more fish near riverbanks and clearer water during certain seasons. “Ten years ago, the river looked tired and empty,” said one long-time resident. “Now you can see life returning. It feels like the river is breathing again.” Environmental scientists caution, however, that recovery is still fragile. Decades of damage cannot be reversed in just a few years, and the Yangtze continues to face pressure from shipping traffic, hydropower dams, and urban wastewater. Climate change adds another layer of risk, with extreme floods and droughts threatening habitats and food chains. Experts say the fishing ban must be paired with stricter pollution controls and smarter water management to ensure long-term success. “Stopping fishing was essential, but it is only one part of the solution,” said a freshwater ecologist involved in river studies. “Industrial discharge, plastic waste, and construction along riverbanks still need to be addressed if the Yangtze is to fully recover.” International conservation groups have praised China’s approach as a rare example of large-scale river restoration driven by national policy. They note that many countries struggle to balance economic growth with environmental protection, and the Yangtze project could serve as a model for other heavily used rivers around the world. The Yangtze River has been central to Chinese civilization for thousands of years, providing water, food, and transport. Its decline in recent decades symbolized the environmental cost of rapid development. Its gradual recovery now represents a shift toward sustainability and long-term planning. While challenges remain, the early results of the fishing ban suggest that strong political commitment and scientific monitoring can bring damaged ecosystems back from the edge. For millions who live along its banks, the Yangtze’s revival is more than an environmental success story—it is a reminder that nature can heal when given the chance.
By Fiaz Ahmed 20 days ago in Longevity
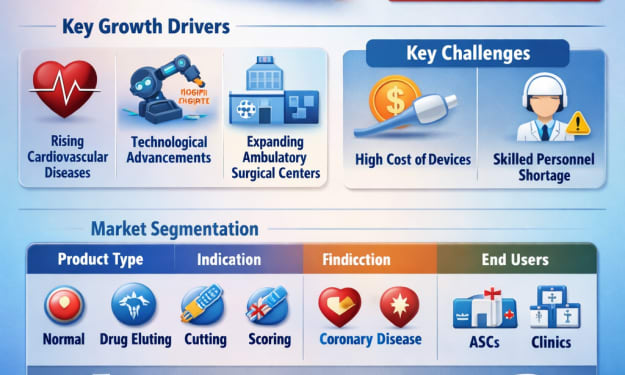
Global Atherectomy Devices Market Size and Forecast 2025–2033. AI-Generated.
Introduction The global healthcare industry is witnessing a steady shift toward minimally invasive procedures, and atherectomy devices are playing a crucial role in this transformation. These specialized medical tools are designed to remove plaque from arteries, restoring blood flow in patients suffering from conditions such as coronary artery disease (CAD) and peripheral artery disease (PAD). With cardiovascular diseases remaining one of the leading causes of death worldwide, the demand for effective, less invasive treatment options continues to rise.
By shibansh kumar20 days ago in Longevity
The Missing Link in Stable Walking: Why Dynamic Stability Matters More Than Strength
When people start noticing changes in their walking, they often assume the problem is muscle weakness or aging joints. While strength plays a role, a lesser-known factor called dynamic stability is usually at the center of the issue. Dynamic stability refers to the body’s ability to stay balanced while in motion — adjusting to shifts in weight, changes in direction and uneven ground.
By AhmedFitLife21 days ago in Longevity