Latest Stories
Most recently published stories in Longevity.
My Husband Has Started a Friendship With a Woman He Used to Work With. Am I Right to Be Worried?. AI-Generated.
When a partner forms a close friendship with someone of the opposite sex, especially someone from their past, it can stir emotions that are hard to ignore. Trust, insecurity, and fear of betrayal can all collide at once. For many spouses, the question is not whether the friendship itself is wrong, but whether the boundaries around it are healthy. A reader recently shared her concern: her husband has reconnected with a woman he once worked with years ago. What began as casual messages has slowly turned into frequent communication—texts, social media interactions, and even plans to meet for coffee. The reader insists she does not want to be controlling, but she cannot shake the feeling that something about the situation feels uncomfortable. This reaction is not unusual. Emotional discomfort does not always mean that something inappropriate is happening, but it does signal that something deserves attention. Why This Triggers Anxiety Friendships with former colleagues are common, but when one of those friendships becomes secretive or intense, it can blur into emotional territory that threatens a marriage. The fear is not always physical infidelity—it is emotional intimacy. Sharing personal problems, private jokes, and daily updates with someone outside the marriage can slowly replace the closeness that should exist between spouses. Experts say jealousy itself is not the enemy. It often points to unmet emotional needs or unclear boundaries. If a spouse feels excluded or dismissed when concerns are raised, the problem becomes less about the friend and more about communication within the marriage. Transparency Matters One of the strongest indicators of whether a friendship is healthy is transparency. Does your husband openly talk about this woman? Does he show you their messages willingly? Or does he become defensive when you ask questions? Healthy friendships survive daylight. If the relationship is innocent, there should be no need for secrecy. Hiding phones, deleting messages, or downplaying how often they talk are warning signs—not proof of cheating, but signals that boundaries may be slipping. Trust is built not only on faith but on behavior. If your partner’s actions create doubt, those feelings deserve to be discussed rather than buried. The Difference Between Control and Boundaries It is important to distinguish between controlling behavior and reasonable boundaries. You are not asking your husband to give up friendships. You are asking for reassurance and respect for your emotional safety. Boundaries might include: Not sharing intimate marital problems with this friend Limiting one-on-one meetings Including you in social settings when possible Being open about communication These are not demands—they are safeguards for the relationship. How to Start the Conversation Approach the topic calmly and without accusation. Instead of saying, “I don’t trust you,” try: “I feel uneasy because I don’t understand what this friendship means to you, and I need reassurance.” This keeps the focus on your feelings rather than placing blame. A loving partner will want to understand your concern, not dismiss it. If he responds with empathy and works with you to find solutions, that is a positive sign. If he mocks your worries or refuses to discuss boundaries, that is a deeper issue than the friendship itself. Self-Reflection Is Also Important Ask yourself what exactly worries you. Is it her specifically? Is it how much time they spend talking? Or is it a sense that your emotional connection with your husband has weakened? Sometimes fear is rooted in past experiences—betrayal, insecurity, or lack of communication. Understanding your own emotions helps prevent the discussion from turning into conflict. When to Seek Help If the tension continues or trust feels damaged, couples counseling can provide a neutral space to discuss expectations and fears. A counselor can help define boundaries that both partners feel comfortable with. Ignoring the issue will not make it disappear. Small doubts can grow into resentment if left unspoken. The Bottom Line You are not wrong to feel uneasy. Your feelings are signals, not accusations. A marriage should be a place where concerns are heard and respected. A friendship outside the marriage is not automatically dangerous, but it becomes problematic when it competes with the marriage for emotional closeness. The real question is not whether your husband should have this friendship, but whether your relationship still feels safe, valued, and prioritized. Trust thrives where openness exists. If both partners protect that trust, friendships do not have to become threats. Sometimes, what seems like a small issue is actually a chance to strengthen communication and reaffirm commitment. Handled honestly and calmly, this moment can bring clarity rather than conflict.
By Fiaz Ahmed 18 days ago in Longevity
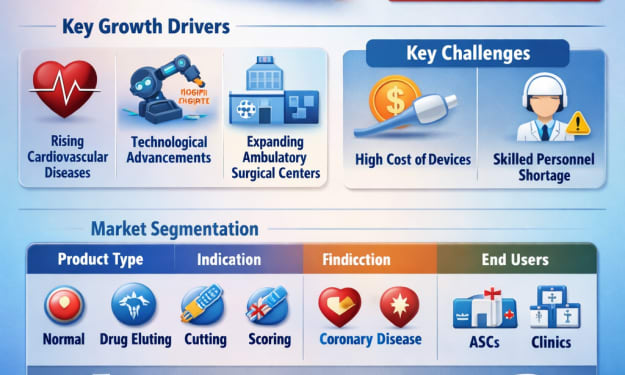
How Robots Are Changing Healthcare
How Robots Are Changing Healthcare One of the most transformative periods in healthcare's history is currently underway. Robotics, which was once mostly associated with manufacturing plants and science fiction, is at the center of this evolution. Today, robots assist surgeons, disinfect hospital rooms, deliver medications, support rehabilitation, and even provide companionship to patients.
By Farida Kabir18 days ago in Longevity
More Than Meets the Eye. AI-Generated.
In an age dominated by instant information and viral headlines, the old adage “things are more than they appear” has never been more relevant. Across politics, technology, social movements, and even everyday life, the reality beneath the surface often tells a story far richer, more complex, and sometimes more troubling than the one initially visible. This week, several events have illustrated that what meets the eye can be only a fraction of the full picture. The Complexity of Global Events Global news often presents headlines that are stark and simple, but the underlying events are frequently layered with nuance. For instance, diplomatic conflicts, trade negotiations, and military movements rarely unfold in isolation. They are shaped by historical grievances, economic imperatives, and cultural undercurrents that may not be immediately obvious. Take, for example, recent tensions in international energy markets. A sudden spike in oil prices may appear to be a simple supply-demand imbalance. However, digging deeper reveals intricate webs of geopolitical strategy, sanctions, and domestic policy decisions. A headline about “rising oil costs” can mask decades of policy, negotiation, and unintended consequences. Social Media and the Illusion of Simplicity Social media has amplified the phenomenon of surface-level perception. Posts, tweets, and viral videos often capture attention with dramatic images or short statements, creating a perception that is easy to digest but incomplete. Complex issues—from global crises to local community disputes—are often distilled into a few words or images, leaving audiences with a partial or even misleading impression. Experts warn that this can foster misinformed judgments and polarized debate. “People tend to respond to what they see, not what they understand,” says a communications analyst. “The first impression becomes the lasting one, even when the underlying reality is far more nuanced.” Hidden Forces in Economics and Finance Economists often emphasize that visible market movements hide deeper forces. Stock market swings, currency fluctuations, and commodity price changes are influenced not just by headline news but also by investor sentiment, algorithmic trading, regulatory shifts, and even subtle policy signals from governments. A sudden drop in a stock index may appear to reflect immediate fear, but the underlying cause could be strategic reallocation by institutional investors or subtle global market trends. Similarly, in emerging economies, inflation rates or shortages of goods may present as a surface-level crisis, but the real story often involves structural issues such as supply chain inefficiencies, domestic policy challenges, and international economic pressures. Understanding the full picture requires digging past the obvious numbers to the human, social, and political factors shaping them. Culture, Media, and Perception Cultural phenomena provide another example of how appearances can be deceiving. Viral trends, public controversies, or celebrity actions may appear simple or superficial, yet they often reflect deeper social dynamics, generational shifts, or ongoing debates about identity, ethics, and values. For instance, a social media controversy about a public figure can reveal long-standing issues around representation, workplace culture, or broader societal expectations. Journalists and media analysts caution that audiences must develop critical thinking to navigate this landscape. “Surface stories grab attention, but real understanding comes from questioning, context, and exploration,” notes a media scholar. Technology and Hidden Layers Even in the realm of technology, appearances can be deceiving. Apps, devices, and platforms that seem straightforward often contain layers of complexity: algorithms that prioritize certain content, data collection practices, and potential security vulnerabilities that are invisible to the average user. Consumers may believe they understand how a tool works based on its interface, but the underlying mechanisms—the architecture, coding, and business model—can have significant implications for privacy, behavior, and decision-making. Artificial intelligence, for example, can appear as a simple tool generating answers or recommendations, but the technology involves enormous datasets, bias considerations, and hidden decision-making rules. The consequences of misuse or misinterpretation may not be immediately visible but can have profound real-world impacts. The Lesson for Individuals and Societies The key takeaway from all these examples is that critical thinking and curiosity are essential. Whether navigating news, technology, finance, or interpersonal relationships, what meets the eye is rarely the full story. Developing the habit of looking deeper, questioning assumptions, and considering hidden contexts allows individuals and societies to make more informed choices. In an era of rapid information, the warning is clear: don’t settle for the obvious. Beneath the visible, there are always layers waiting to be understood, connections waiting to be made, and implications waiting to be recognized. As this week has demonstrated across multiple arenas—news, culture, finance, and technology—life is almost always more than meets the eye. Those who understand that reality have a better chance of navigating the complexities of a fast-moving, interconnected world.
By Fiaz Ahmed 18 days ago in Longevity
Lindsey Vonn Has Another Surgery After Olympic Crash, Says She’s Returning to U.S.. AI-Generated.
American skiing legend Lindsey Vonn is set to return to the United States following a recent surgery, the latest in a series of medical interventions after a high-speed crash during the Winter Olympics. The 38-year-old athlete, widely regarded as one of the greatest alpine skiers of all time, confirmed the update on social media, assuring fans that she is recovering steadily and focusing on rehabilitation. Crash at the Olympics Vonn’s crash occurred during the downhill skiing event at the 2026 Winter Olympics, sending shockwaves through the sporting world. Footage from the event showed Vonn losing control in a challenging section of the course, resulting in a fall that left her with multiple injuries, including damage to her knee and upper body. Medical teams immediately assessed her condition, and she was transported to a nearby facility for treatment. Despite the severity of the incident, Vonn demonstrated remarkable composure, communicating with her team and the media to reassure fans that she would focus on recovery. A Series of Surgeries This most recent procedure marks the third surgical intervention since the Olympic crash. According to her team, the surgery addressed lingering complications that were affecting her mobility and strength. While her doctors had initially hoped that physical therapy alone could restore function, it became clear that surgical intervention was necessary to prevent long-term issues. “Lindsey is incredibly resilient,” said her orthopedic surgeon. “Her determination to return to full health and maintain her active lifestyle is exceptional. This surgery is a precautionary step to ensure that she can recover fully and avoid further injury.” Vonn’s previous surgeries following the crash included repair of a torn ligament in her knee and minor procedures to address bruising and fractures sustained during the fall. Recovery from each operation required careful monitoring, pain management, and intensive physiotherapy. Returning Home In her statement, Vonn confirmed that she would be returning to the U.S. to continue her recovery in a familiar environment. “Being home will allow me to focus on rehabilitation, spend time with family, and work with my team of therapists to get back to full strength,” she wrote. Fans and fellow athletes have expressed their support across social media platforms. Many highlighted her career achievements, including four World Cup overall titles, Olympic medals, and her record-breaking performances in speed events. Supporters noted that Vonn’s dedication to her sport and ability to overcome injury serve as an inspiration to athletes of all ages. Long-Term Recovery and Future Plans Although Vonn has not confirmed whether she intends to return to competitive skiing, her focus in the short term is clear: regaining strength and mobility. Experts indicate that recovery from multiple surgeries, particularly involving the knee and major muscle groups, can take several months. “Rehabilitation will be gradual and carefully structured,” said her physiotherapist. “We are looking at a combination of strength training, flexibility exercises, and low-impact cardiovascular activity. Lindsey’s motivation and discipline make her an ideal candidate for a successful recovery.” Vonn has previously endured serious injuries during her career, including torn anterior cruciate ligaments (ACL) and fractures. Each time, she has managed to return to top-level competition, demonstrating her resilience and commitment. Reactions from the Skiing Community Prominent figures in the skiing world have voiced their support for Vonn’s recovery. Fellow Olympians, coaches, and international ski federations sent messages praising her courage and offering encouragement. “Lindsey embodies the spirit of alpine skiing,” said a member of the U.S. Ski & Snowboard leadership team. “She competes with passion, overcomes adversity, and inspires the next generation. We look forward to seeing her back on her feet and enjoying life to the fullest.” Sports analysts note that while Vonn may be stepping back from competitive events for the foreseeable future, her influence on skiing remains profound. She has advocated for athlete safety, mental health awareness, and support for women in sports, contributing to the evolution of alpine skiing culture. Looking Ahead For now, Vonn’s priority is her health and rehabilitation. Fans around the world continue to follow updates on her progress, expressing admiration for her courage and perseverance. As she returns to the United States, her team remains focused on ensuring she receives the best care and support possible. “This isn’t the end of my journey,” Vonn wrote in her statement. “It’s just another chapter. I am determined to heal, stay positive, and embrace the future with strength and gratitude.” With multiple surgeries behind her and a dedicated support team in place, Lindsey Vonn’s path to recovery reflects both the challenges and resilience inherent in elite sports. Her return to the U.S. marks the beginning of this next phase—a phase focused on health, family, and the enduring love of skiing.
By Fiaz Ahmed 18 days ago in Longevity
“Nothing Says Love Like Chemicals”: Valentine’s Roses Often Covered in Pesticides, Testing Finds. AI-Generated.
Valentine’s Day roses may look romantic, but new testing shows many bouquets come with an unwelcome extra: high levels of pesticide residue. Consumer advocates say the findings highlight a largely hidden problem in the global flower industry, where heavy chemical use is common and regulation remains uneven. A recent investigation by the Environmental Working Group analyzed roses purchased from major retailers in several U.S. cities ahead of Valentine’s Day. Laboratory tests detected traces of more than a dozen different pesticides on some flowers, including chemicals restricted or banned for use on food crops. While roses are not eaten, researchers warn that frequent handling — by florists, warehouse workers, and consumers — can still pose health risks. “People associate roses with love and celebration, but what we found was a cocktail of chemicals,” said an EWG spokesperson. “These pesticides don’t disappear when the flowers are cut. They remain on petals and leaves that people touch and bring into their homes.” Most roses sold in the United States are imported, primarily from Colombia and Ecuador, where large-scale flower farms rely on intensive pesticide spraying to meet demand for flawless blooms. Industry experts say pests and fungal diseases thrive in the humid greenhouse conditions used to grow roses year-round, making chemical control the cheapest and fastest solution. Testing found residues of fungicides and insecticides commonly used in commercial flower production. Some of these substances have been linked in scientific studies to hormone disruption, respiratory problems, and skin irritation. Although the amounts detected were within legal limits for ornamental plants, advocates argue that safety standards for flowers are far weaker than those for fruits and vegetables. The U.S. Department of Agriculture does not regulate pesticide residues on cut flowers in the same way it monitors food products, because roses are not intended for consumption. This regulatory gap means consumers rarely receive information about what chemicals were used to grow the flowers they buy. Florists are among the most exposed. Many handle thousands of stems daily in the days leading up to Valentine’s Day. “We’ve had workers complain about headaches and rashes during peak seasons,” said a shop owner in New York who asked not to be named. “We wear gloves now, but customers don’t think about that when they’re holding a bouquet.” Environmental groups also point to the impact on farmworkers in exporting countries. Reports from labor organizations describe frequent pesticide exposure, limited protective equipment, and long working hours during the Valentine’s rush. “The health burden is not shared equally,” said a labor rights advocate based in Bogotá. “Those growing the flowers face the highest risks.” The flower industry disputes that roses pose a danger to consumers. Trade associations maintain that approved pesticides are used according to safety guidelines and that exposure levels are minimal. “These products are essential to protect crops and ensure quality,” said a representative of a major floral exporter. “Without them, we could not meet global demand or control disease outbreaks.” Still, demand for alternatives is growing. Organic and “pesticide-free” roses are becoming more available, though they are often more expensive and harder to source in winter. Some florists are shifting to locally grown flowers or encouraging customers to buy potted plants instead of cut roses. Health experts recommend simple precautions: washing hands after handling flowers, keeping bouquets away from food preparation areas, and avoiding sleeping with flowers near pillows or beds. Removing outer petals and using gloves when arranging bouquets can also reduce exposure. For consumers, the findings challenge the image of roses as a harmless symbol of romance. “It’s ironic that a gift meant to express care may come with chemical risks,” said the EWG spokesperson. “We’re not saying people should stop buying flowers. We’re saying they deserve transparency and safer choices.” As Valentine’s Day sales continue to soar each year, advocates hope the spotlight on pesticides will push regulators and retailers toward stricter standards. Until then, the classic bouquet may carry a hidden message alongside its petals: love, wrapped in chemicals.
By Fiaz Ahmed 18 days ago in Longevity
Best Supplements For Weight Loss for Women
The best supplements for weight loss for women typically include fiber supplements, green tea extract, probiotics, and metabolic support compounds like berberine. They work best when combined with calorie control, exercise, and hormone balance support — not as stand-alone “fat burners.”
By Edward Smith19 days ago in Longevity
FridaBaby Faces Backlash Over Alleged Sexualized Marketing of Infant Products
The baby-care brand FridaBaby, known for products such as the NoseFrida nasal aspirator and infant thermometers, is facing a surge of online backlash following the resurfacing of old marketing materials featuring suggestive and sexualized language. Social media users have widely circulated screenshots of posts and product packaging, criticizing the brand for content deemed inappropriate for items designed for infants.
By Story Prism20 days ago in Longevity
James Van Der Beek’s Colon Cancer: A Warning for Young Adults
The sudden news of James Van Der Beek’s death at 48 shocked fans worldwide, not just because of the loss of a beloved actor, but also because it highlights a growing public health concern: colorectal cancer in younger adults. Best known for his roles in Dawson’s Creek and Varsity Blues, Van Der Beek’s journey with stage-3 colorectal cancer underscores the importance of recognizing subtle symptoms, seeking early medical evaluation, and understanding that cancer is not limited to older adults.
By Story Prism20 days ago in Longevity