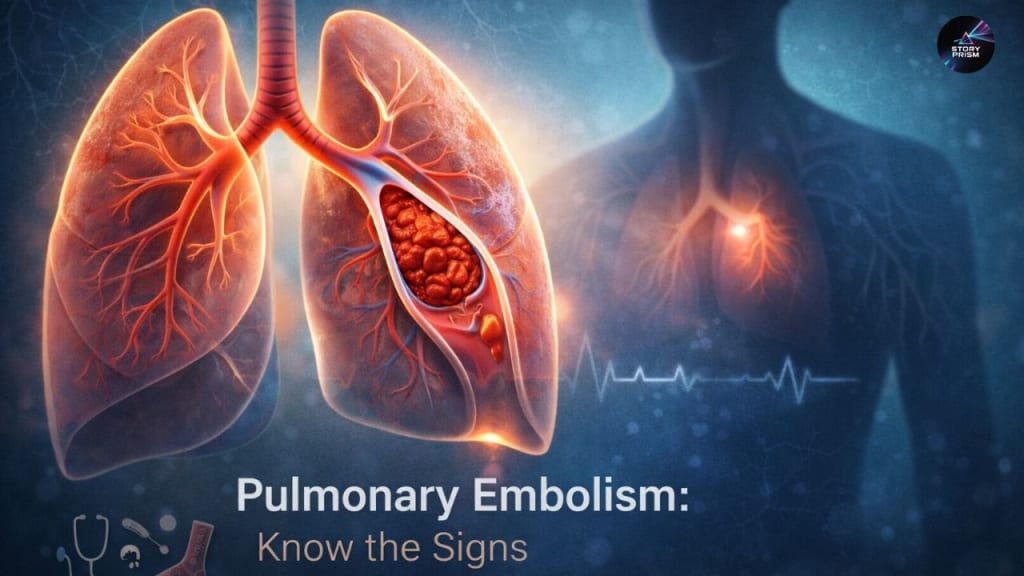
Pulmonary Embolism: Symptoms, Causes, Treatment, and Prevention of a Silent Killer
Understanding the Silent Killer: Early Signs, Risk Factors, and Life-Saving Treatments for Pulmonary Embolism
Introduction
Pulmonary embolism (PE) is a serious, potentially life-threatening condition that occurs when a blood clot blocks one or more arteries in the lungs. It is one of the most critical emergencies in cardiovascular health, ranking just after heart attacks and strokes in terms of morbidity and mortality. PE often originates from deep vein thrombosis (DVT), a blood clot in the veins of the legs or pelvis, that travels through the bloodstream to the lungs. Understanding the risk factors, early symptoms, diagnostic methods, treatment options, and preventive strategies is essential to improving outcomes and saving lives.
Despite advancements in medical technology, pulmonary embolism remains underdiagnosed due to its sometimes subtle and nonspecific symptoms. Early recognition and timely intervention are critical, as untreated PE can rapidly progress to severe complications, including pulmonary hypertension, heart failure, and death. In this article, we provide a comprehensive overview of pulmonary embolism, drawing on clinical insights from leading medical institutions and research studies.
What is Pulmonary Embolism?
Pulmonary embolism is the obstruction of a pulmonary artery or one of its branches by a thrombus (blood clot), fat, air, or tumor fragments. Most cases are caused by thromboembolic events originating in the deep veins of the lower extremities (DVT), which then dislodge and migrate to the lungs. When the embolus lodges in the pulmonary circulation, it restricts blood flow to lung tissue, resulting in ventilation-perfusion mismatch, hypoxemia, and right ventricular strain.
Types of Pulmonary Embolism
PE can vary in severity and location:
1. Massive PE: Involves a large clot obstructing the main pulmonary artery or multiple branches. Often results in hemodynamic instability, shock, or sudden death.
2. Submassive PE: Affects intermediate-sized pulmonary arteries, causing right ventricular strain without significant hypotension.
3. Segmental or Subsegmental PE: Smaller clots may involve segmental or subsegmental arteries. Symptoms are often subtle or even absent but can progress if left untreated.
Etiology
The majority of PEs originate from DVT in the lower extremities. Less common sources include:
• Fat emboli from fractures of long bones
• Amniotic fluid emboli during childbirth
• Air emboli, usually from medical procedures or trauma
• Tumor emboli
Risk Factors for Pulmonary Embolism
PE develops when blood clots form due to conditions described by Virchow’s triad:
1. Venous stasis: Reduced blood flow due to immobility, bed rest, or prolonged travel.
2. Hypercoagulability: Increased tendency of blood to clot, which can result from genetic clotting disorders, cancer, pregnancy, or hormone therapy.
3. Endothelial injury: Damage to blood vessel walls caused by trauma, surgery, or inflammation.
Specific Risk Factors Include:
• Age: Individuals over 40 have increased risk.
• Previous history of DVT or PE
• Surgery or trauma: Particularly orthopedic or pelvic surgery.
• Immobility: Bed rest, long flights, or sedentary lifestyle.
• Cancer and chemotherapy
• Pregnancy and postpartum period
• Hormonal therapies: Oral contraceptives or estrogen therapy
• Obesity and smoking
• Central venous catheters
Symptoms of Pulmonary Embolism
Symptoms of PE can vary widely, making early diagnosis challenging. While some patients exhibit acute, life-threatening symptoms, others may have subtle signs that mimic less severe conditions.
Common Symptoms
• Sudden shortness of breath
• Sharp, stabbing chest pain, worsened by deep breathing (pleuritic pain)
• Rapid heartbeat (tachycardia)
• Rapid breathing (tachypnea)
• Coughing, sometimes with blood-streaked sputum
• Dizziness, lightheadedness, or fainting (syncope)
• Sweating and anxiety
• Pale, clammy, or bluish skin (cyanosis)
Signs of DVT
Because PE often originates from DVT, recognizing leg clot symptoms is crucial:
• Swelling in one leg
• Pain or tenderness, especially when standing or walking
• Warmth or redness in the affected leg
• Visible enlarged veins
Complications of Pulmonary Embolism
Pulmonary embolism can result in severe complications if untreated or if treatment is delayed. Some of the most serious complications include:
• Pulmonary hypertension: Chronic blockage increases pressure in the pulmonary arteries, causing long-term right heart strain.
• Right ventricular dysfunction or heart failure: The heart struggles to pump blood through obstructed pulmonary arteries.
• Death: Especially in massive PE.
• Recurrent PE: Patients with one episode are at increased risk for future clots.
Diagnosing Pulmonary Embolism
Accurate diagnosis is critical due to the nonspecific nature of PE symptoms. Physicians typically use a combination of clinical assessment, imaging studies, and laboratory tests.
1. Clinical Assessment
• History and physical examination
• Risk assessment scores: Wells Score, Revised Geneva Score, and PERC criteria help estimate the likelihood of PE.
2. Laboratory Tests
• D-dimer: Elevated levels suggest active clotting but are nonspecific. Useful for ruling out PE in low-risk patients.
• Blood gas analysis for oxygenation and acid-base status.
3. Imaging Studies
• CT Pulmonary Angiography (CTPA): First-line diagnostic tool. High sensitivity and specificity for pulmonary emboli.
• Ventilation-Perfusion (V/Q) scan: Used when CT is contraindicated.
• Pulmonary angiography: Considered gold standard in certain complex cases.
• Duplex ultrasound of the legs: Detects underlying DVT.
4. Supportive Tests
• Electrocardiogram (ECG): May show sinus tachycardia or right heart strain patterns.
• Echocardiography: Evaluates right ventricular function in severe PE.
Treatment of Pulmonary Embolism
Treatment depends on the severity of PE, underlying risk factors, and patient stability. The primary goal is to stop clot growth, dissolve existing clots, and prevent recurrence.
1. Anticoagulation (Blood Thinners)
• Heparin, low molecular weight heparin, warfarin, and newer direct oral anticoagulants (DOACs) prevent clot extension and recurrence.
• Typically continued for 3–6 months, with longer durations for high-risk patients.
2. Thrombolytic Therapy
• Clot-dissolving drugs (e.g., tPA) used in massive PE or hemodynamically unstable patients.
• High risk of bleeding; reserved for severe cases.
3. Catheter-Based Interventions
• Catheter-directed thrombolysis or thrombectomy for targeted clot removal.
• Minimally invasive, used in patients at risk of bleeding from systemic thrombolysis.
4. Surgery
• Pulmonary embolectomy is reserved for life-threatening PE unresponsive to other treatments.
5. Inferior Vena Cava (IVC) Filters
• Placed in patients who cannot take anticoagulants to prevent further emboli from reaching the lungs.
Prevention of Pulmonary Embolism
Prevention strategies are crucial, especially for high-risk individuals:
• Regular physical activity and leg exercises during long travel
• Compression stockings to improve venous return
• Early ambulation after surgery or illness
• Maintaining a healthy weight and avoiding smoking
• Appropriate use of anticoagulants in at-risk patients
• Hydration to reduce blood viscosity
Living With Pulmonary Embolism
Recovery after PE varies depending on severity and overall health. Patients often require:
• Follow-up anticoagulation therapy
• Monitoring for signs of chronic pulmonary hypertension
• Lifestyle modifications to reduce recurrence risk
• Awareness of bleeding risks associated with anticoagulants
• Psychological support, as PE can cause anxiety and fear of recurrence
Conclusion
Pulmonary embolism is a medical emergency that can strike silently yet have devastating consequences. Awareness of risk factors, early symptoms, and preventive measures can significantly improve outcomes. Modern diagnostic tools and treatments, from anticoagulation to advanced catheter-based interventions, have transformed PE management, yet early recognition remains critical.
Educating patients, caregivers, and healthcare providers about PE symptoms and risk factors, combined with timely medical intervention, is the most effective strategy to reduce mortality and long-term complications. Whether through preventive measures, early detection, or aggressive treatment of acute cases, pulmonary embolism is a condition that can be managed successfully with comprehensive, evidence-based care.






Comments
There are no comments for this story
Be the first to respond and start the conversation.