A Study on Psychosomatics
When Physical Injuries Are Caused by Mental Disabilities, and Why
In order to properly begin this study, I must first define the term “psychosomatic” so you, as the reader, are familiar with its meaning. The official definition from the Merriam-Webster dictionary is as follows:
- of, relating to, concerned with, or involving both the mind and the body
- of, relating to, involving, or concerned with bodily symptoms caused by mental or emotional disturbance
The word psychosomatic is translated to mind (psyche) and body (soma). That is an accurate name considering all psychosomatic disorders are diseases of the mind and body, involving both. (Should a disorder involve only one, it would not be classified as psychosomatic. Instead, it would simply be a physical injury or a mental illness.) Psychosomatic injuries are seen in everyday life; almost everyone can recall experiencing a headache brought on by stress. Other normal symptoms include nausea, back or chest pain, dizziness, fatigue, or decrease in appetite. The common causes tend to be little things like stress, guilt, feelings of failure, waves of sadness, or just nerves in general. However, just as mental illnesses can be far more urgent than a simple bout of momentary anxiety, psychosomatic disorders can be much worse. This research paper has been written to focus on educating you, as the reader, on the topic that is psychosomatic disorders.
Introduction to Psychosomatics
To introduce you to the subject, I will bring up a case most of us are familiar with, and that is the psychosomatic experience of Dr. John Watson in the television show Sherlock. In the first episode, Watson struggles to walk from a leg injury, but it is later revealed that he had been suffering from a physical injury as a result of PTSD. Whilst that is a fictitious situation, it is an accurate portrayal of how psychosomatic disorders work.
Stress, depression, and anxiety are the three most common mental issues connected with those who are psychosomatic. Because those three symptoms can be triggered by certain situations, the physical injury accompanying the mental sickness will often be more severe at one time or another, depending on the mood or environment of the affected person. For instance, if someone is suffering from chest pains connected to anxiety, they might feel little to no pain until the anxiety starts to act up. The mental and physical disorders are directly connected in almost every situation.
When a person is complaining of an injury, but tests disprove that the root of the problem is a physical issue, and they experience a mental disorder that can be connected to said injury, they are diagnosed as psychosomatic. However, even though many cases of psychosomatic disorders have been recorded, it is not yet proven exactly how the injuries develop. For obvious reasons, that is very difficult to prove. All we know for sure is that they are indeed connected to mental illnesses, and we have yet to learn anything beyond that with our studies. Supporting evidence of the aforementioned statement is that some people have been in war and sustained no injuries, until the mental game had begun. (Oftentimes, the injuries will start to affect them only after they return home.) The things that they see and experience affect their mental health, correlating to their physical health in turn. Many war veterans and survivors of trauma are diagnosed with PTSD, which can be connected to psychosomatic disorders in some instances.
People suffering from psychosomatic injuries often believe the illness is purely physical, denying when they are told it originated from a psychological issue. Because they accept the disease (whether they strongly hate it or just complain), it continues to affect them. Most people who deny that the disorder is psychological, refuse treatment options that help to improve mental health, and in some cases, no conditions, physical or mental, improve.
The Classifications
Somatization is the correct word to use when describing physical symptoms caused by psychological or emotional factors: simple things like, those mentioned in our Definition. Somatoform disorders (or somatic symptom disorders, as they were retitled in 2009) are far worse in comparison. They are the extreme end of the wide spectrum, a diagnosis given when there is a terrible physical condition, and no explanation. The official classification for such a diagnosis is under the category mental health. People affected are often described as very emotional, especially about their symptoms.
Hypochondriasis is one of such disorders. However, it may or may not affect the physical, worse than it already is. People affected by hypochondriasis have the overwhelming fear that minor problems, like headaches or leg pain, are symptoms of a bad disease, such as cancer. For example, one might fear that a stomachache is a symptom of an internal disorder. They often waste time obsessively worrying over their symptoms, and will spend a lot of money going to get tests done. If one doctor tells them that nothing is wrong, they will often go to a different doctor, fearing that the first might have missed something. This disorder is not quite like the others, and, in turn, treatments can vary.
Conversion disorder is the most common besides somatization disorder. It is the classification for psychosomatic symptoms that suggest a serious disease, such as blindness, deafness, or paralysis. The symptoms often develop quickly, over a few days or even hours, responding to a stressful or traumatic situation. The symptoms usually don’t last too long, only for a few weeks or less except in serious cases. There is no telling if the disorder will affect the patient just once, or if it will return. (In a lot of cases, it comes and goes). This would be the disorder that Dr. John Watson would have suffered from, in our example a few paragraphs ago: after returning home from war, his leg would have been partially paralyzed, and most likely also in some pain.
Body dysmorphic disorder is a common somatization seen in teenagers and young adults. It appears in people that worry about their body appearance more than average, to the point where they notice the tiniest flaws, and might even ponder the possibility of surgery to fix it. Sometimes this is linked to bulimia or anorexia, but those are often put in a different category. However, both bulimia and anorexia are linked back to mental conditions, because it is rarer to find a case that is purely physical. A lot of anorexia cases involve bullying, whether it be inflicted by peers or by family. As it was mentioned before, the disorder is mostly seen in teenagers or young adults, and women are affected more than men by a big percentage. (While it has been seen in boys before, women statistically seem to suffer from low self-esteem more than men.)
Pain disorder is the final classification we will list here. It is fairly self-explanatory: the person suffers from persistent pain, that cannot be traced back to anything physically happening in the body, and is therefore credited to the brain. The pain can be extreme, or it may be just an uncomfortable feeling. It also varies in where it affects each patient—some people might complain about their legs, while others may suffer in their whole body. In rare cases, the pain will be based internally, and it may be mistaken for a disorder of the organs. The symptoms will come and go, as they do in most somatoform disorders.
Diagnosis
In years past, there have been more requirements in order to diagnose someone with a psychosomatic disorder. People used to require a history of at least eight symptoms (including four pain symptoms and two gastrointestinal symptoms) to be considered for official diagnosis, according to the DSM-IV. However, there are not many cases of psychosomatic illnesses, because they are rare disorders and therefore scientists and psychologists have made the diagnosis less restrictive, requiring only four somatic symptoms in men, and six in women, with no requirements on what those symptoms may be. (However, they prefer that the patient show signs of a gastrointestinal issue, because that is common with these types of disorders). Yes, men require fewer symptoms to be diagnosed, but the system isn’t entirely unfair: women suffer from somatic symptoms more, on average, so a woman would be in the same condition as a man at a four-to-six ratio.
Treatments
After diagnosis comes the extensive treatment process. Whilst the treatment for all types of psychosomatic disorders can vary, based on the cause and the effect, they tend to have one thing in common, and that is the fact that it can be difficult to treat certain patients or certain symptoms. Oftentimes, people with somatoform illnesses will reject the diagnosis, and therefore reject the treatment. Substance abuse can be one of the issues accompanying the illness, and it can be difficult to give the person any medication because of that: some medications warn against drinking alcohol while taking.
Treatments often involve talking about the symptoms, and identifying mental health issues that the person struggles with. Counseling is always an option that psychosomatic patients are given. Cognitive behavioral therapy may or may not help improve the patient’s health. For those struggling with body dysmorphic disorder, or pain disorder, the instruction to begin taking selective serotonin reuptake inhibitors (SSRIs) may be prescribed. SSRIs are antidepressants used to treat bulimia nervosa, panic disorder, obsessive-compulsive disorder, and depression. By targeting depression, the SSRIs can often reduce the symptoms that are caused by that mental illness, and begin to improve the corresponding psychosomatic disorder.
Some other types of psychotherapy have been used in an attempt to try and help people that have been affected, but nothing has been proven to work yet. Some doctors continue to study somatic disorders so they might discover an easier or more effective treatment method. While there is no shortage of ideas to try, proving that the ideas actually work is much more difficult. Because of this, cognitive behavioral therapy and antidepressants (in some situations) remain the number one treatment methods for those who are diagnosed as psychosomatic.
Psychosomatics in Children
The developmental stage of a child is, by far, the worst time that anyone could begin to show symptoms of somatic issues. A delay to diagnose the disorder, especially with children, can extend the length of treatment significantly. If the issues persist without treatment, it can set the child up for much worse problems, as they transition through puberty, and into adulthood. Children are also more likely to be affected by the reactions of others to the illness, which may worsen conditions.
Somatoform symptoms are fairly common in children, but cannot be diagnosed, because they lack a specific symptom necessary to classify it. When children are diagnosed, they are typically treated with behavioral, or relaxation techniques, and/or family therapy.
In an Oxford case study, an eleven-year-old girl was struggling with pain disorder and paralysis. She did not suffer from anxiety or depression, but she had experienced a recent athletic failure. (Feelings of failure in extracurricular or scholastic activities have been seen to affect psychosomatics all ages, but diagnosis is usually seen in children.) The eleven-year-old had also recently learned that a family friend had been abusing her older sister. She started experiencing bouts of pain, that led to paralysis in the lower half of her body. She stayed home from school for months on end, falling behind in her work. Her condition did not improve with her parents’ constant panic, always rushing around her. In a psychosomatic situation, especially with children, panic or fear from loved ones can halt improvements or even make things worse.
After weeks of enduring the pain and temporary paralysis, she lost complete use of her legs. This caused her parents to rush her to the hospital, where she was put in a room for a few days so tests could be run. After finding no physical disease that was the root of the problem, she was diagnosed as psychosomatic with pain disorder, and conversion disorder. She immediately began treatment, with cognitive therapy. It was noted, during her stay at the hospital, that she would often joke around with the hospital staff, as if nothing was wrong, and that her symptoms seemed to improve as her spirits lifted. The months of panic, fear, and stress had taken its toll on her condition, but she began to thrive once more. A few weeks later she was allowed to go back home and return to the hospital only a few times for checkups, which got less and less frequent as time passed. She could not run or exert herself physically for a week or two, but soon she was playing sports again, as she had been before. She returned to school, and the symptoms never returned.
That case study is just one of many that have been recorded over the past years. I have included it because it seems fitting and is a good representation of what often happens in the lives of somatoform-affected children. When the parents, relatives, and friends of the child stay calm, the patient is less likely to worsen in condition. Seeing a doctor is also crucial to halting the disorder from continuing to affect the child. In the case study, it would have been a lot more beneficial, for both the child and her family, had they gone to the hospital before she lost all the feeling in her legs, not after. She was already suffering from the pain disorder and had a difficult time sleeping at night, yet it was allowed to continue. While medications might have helped her physical symptoms for a certain time period, a psychosomatic illness is just one example of a disorder that requires treatment besides just pills.
It should be noted that one of the most common causes of somatoform disorders in children is bullying, whether it is by peers, teachers, or family. There have been many instances of psychosomatic symptoms found in children who struggle with depression and low self-esteem, as a result of bullying. While bullying is just one cause of mental illnesses, I felt the need to state that it does indeed affect a child’s health, and that it is the worst possible time in someone’s life it could happen. In rare cases, some children diagnosed with somatization have been pulled from school to pursue the homeschooling route, and their symptoms improved as their surroundings were more positive throughout their developmental stage.
PTSD and Psychosomatics
Another cause of somatization is post-traumatic stress disorder. Depression, anxiety, dissociation, and negative affectivity can be a part of PTSD. The somatic symptoms experienced by survivors of trauma are sometimes described as unexplained, since there aren’t many studies involving this category. (There are many studies on somatic tendencies in everyday life and with those suffering from depression, stress or anxiety, but there seems to be a shortage of information when involving the category of trauma.) Despite the lack of reports, it is no lie that we can see psychosomatic symptoms showing up in the lives of those who have lived through war or have experienced trauma throughout the years.
To show an example of this, I read an article that surveyed 169 Danish men and women who survived a series of explosions in a firework factory, whether they were working or simply in the surrounding area. This event happened in a residential area in the afternoon hours of November 2004, but no children were surveyed. (It is possible that the children may have been at school and missed the event. Regardless of where they were, though, this study does not focus on a younger age group.) The explosion measured a 2.2 on the Richter scale, and around 260 houses were partially or completely destroyed. The damages were estimated to cost millions of dollars, but the mental damages might have been far more traumatic for those in the area.
The 169 people surveyed, took questionnaires both three months and one year after the event. Out of the 169, 13 percent could be diagnosed with PTSD, and 27 percent could be diagnosed with sub-clinical PTSD (lacking just one symptom needed to diagnose full PTSD). Out of those diagnosed, only a fraction of them could have been officially psychosomatic. This study is limited because it not only surveys a group of less than two hundred, but it also limits the traumatic factor to the factory explosion. In comparison, childhood trauma leading into adulthood is much more likely to end up showing somatic symptoms, and veterans who return from war have a higher average of diagnosis (especially if involved with torture or interrogation). The one thing that the study did prove was the already-known fact that somatization disorders are very rare, even in cases involving things such as post-traumatic stress disorder.
The Most Common Somatization
Out of the five somatic disorders, the one simply titled somatization disorder is the most common. It has a more broad definition, so it makes sense that more people are affected by it. As we talked about before, somatization is when the somatic illness becomes a disorder, no longer just stress headaches or anxious chest pains. Even though I have written that it is a category of its own (which it is), all of the other disorders can also be classified as a somatization disorder because of their nature. (However, we have the other titles for a reason, and we use them.)
The second most common somatization is conversion disorder. On average, we see a few hundred cases in the US per year, and the majority of them are women.
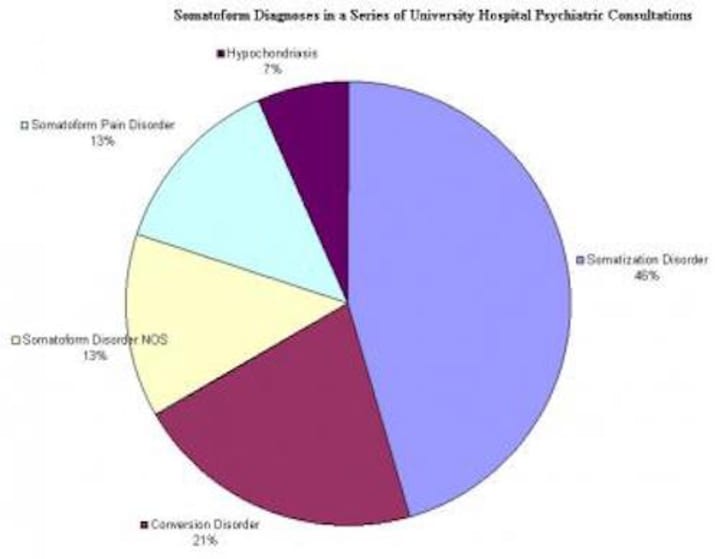
A few university hospitals decided to do a group study on the somatic illnesses people were suffering from. Oxford reported the study after the research was complete. The graph above depicted the different types of psychosomatic disorders, and their percentages, in terms of how they relate to each other, and how often they are diagnosed. As expected, hypochondriasis is the most rare of the group, claiming only 7 percent of all patients. It seems fairly accurate that it isn’t as common—not many people are that intensely paranoid. The study did not include body dysmorphic disorder.
The reason that somatization disorder claims the highest percentage of diagnosable patients per year is because it has the broadest diagnosis spectrum. In conversion disorder, one must have experienced some type of paralysis or hearing/sight loss in order to be officially diagnosed, along with the four or six symptoms (depending upon the gender). With somatization disorder, the only requirement is the four or six symptoms.
Of course, there are common cases of people experiencing more than one disorder at the same time. As we mentioned before, Dr. John Watson would have been suffering from both conversion and pain disorders. The eleven-year-old girl we discussed was affected by the same. When conversion and pain disorders are combined, it is the most difficult to tell psychosomatic illnesses apart from something actually serious. (Whenever someone has paralysis or sight loss and pain, it usually means that there is something wrong with the physical body, not a mental issue.)
There are other combinations of two or more disorders, but they will remain unmentioned as they do not fit into anything else we have previously discussed. It would be irrelevant to introduce another case study, after we have already done two with different outcomes, not to mention that it would require your attention for something we have covered.
The History of Psychosomatics
In the past, there are hardly any reports of psychosomatic disorders. This is mostly because, before the late seventies and eighties, doctors and scientists did not recognize what a psychosomatic illness was. Back then, with the lack of technology we use in this day and age to diagnose and run tests, there was no way to tell if the disorder was physical or mental. Because of that, disorders like that were treated like physical diseases and labeled chronic if they were not cured.
However, today is a different story. We can now diagnose these kinds of things fairly easily, and doctors know the proper questions to ask to provide them with enough information to diagnose. Not only that, but some of the public are aware of these types of disorders. Of course, because of their rarity, not everyone knows they exist, but that has never proved to be an issue. All it takes is a simple explanation and people seem to understand.
One could say that the rate of psychosomatic patients has risen over the past few years, but the argument can be made that it is because we have just now gained the ability to diagnose them. In the past, there were hardly as many cases, but that is because they were simply treated like any physical injury. In some lucky instances, patients got better from the use of medication.
A study was done in Taiwan by some medical professionals and doctors, who were wondering if psychosomatic cases had become more common. They took numbers from the past years and compared them, and found that the rate of somatic disorder diagnosis had risen significantly. It was not stated if they put the information to use, or if they just studied it so they might have it later if it became necessary. There was an increase in somatic disorders as compared to the years before. Over the twelve years, Taiwan saw an increase in the appearance of the disorders, a difference of a little under four thousand cases per one hundred thousand citizens. The biggest jump was from 1998 to 1999, with a number that was just a little over two thousand. There was no information regarding the continued study of Taiwan’s clearly affected population, but it does prove one thing—we are seeing higher percentages of cases developing as the years continue. There is no telling if this will continue to remain true as we now have better treatment options available than we did back then. The introduction of SSRIs to the treatment process has targeted the depression symptoms that many patients suffer from. Regardless, psychosomatic disorders tend to be difficult to treat and complained about by many, despite their rarity.
Conclusion
Whether a psychosomatic disorder plagues an adult or a child, men or women, it is one of the most unpleasant experiences one can go through. Those who have experienced it first, and do their best to continue therapy and go through regular checkups to make sure it doesn’t happen again, and the family and friends of patients are always encouraging the affected person to continue taking care of their health. No mental illness or physical disorder is fun to suffer through, but a combination of the both is more than most people can handle. A lot of times, the fact that the illness is both mental and physical traps them in a cycle: depression brought on by a physical ailment, and a physical ailment affected by the depression. (It is then that doctors recommend SSRIs or other antidepressants to the patient. Of course, never consider a medication unless your doctor prescribes it—many times, people believe they require a certain medication when it is the wrong choice for their situation.)
Psychosomatic disorders are no joke, but that is not news. No disorder should ever be taken lightly. This is just one of many that affect us as humans, and we have learned how to better take care of our bodies when diagnosed. We are always improving medically, and I have a feeling that this will be no different. In the future, there will be more effective medications designed to target the mental illness and directly improve the physical, but we are not there yet. Who knows how long it may be until we see a better breakthrough, and who knows who might contribute to the research? One thing is for certain, though. Our future is destined to be better.
About the Creator
Em Jenkins
feminist. climate change activist. supporter of march for our lives. proudly advocating equality for all. film major. future president of the united states of america. just trying to share what i know and learn what you have to tell me!





Comments
There are no comments for this story
Be the first to respond and start the conversation.