The Unsung Heroes Holding Up Your Bladder: A Deep Dive Into What Keeps You Dry (and Sane!)
You're doubled over laughing at a friend's terrible joke, or maybe you're mid-sneezing fit thanks to spring pollen, and suddenly...
Ever had that moment? You're doubled over laughing at a friend's terrible joke, or maybe you're mid-sneezing fit thanks to spring pollen, and suddenly... panic. That urgent, internal whisper: "Hold it together! Don't leak!" We've all been there. It's a universal human experience, tied directly to that humble, balloon-like organ – the urinary bladder. But have you ever stopped to wonder, especially in those precarious moments, what are the supports of the urinary bladder that keep everything, well, contained?
It’s easy to take this silent workhorse for granted. We fill it, we empty it (hopefully at appropriate times!), and rarely give a second thought to the intricate scaffolding holding it securely in place. Yet, understanding this hidden support system isn't just anatomy trivia. It’s key to appreciating our bodies, preventing problems, and maybe even sparing ourselves some embarrassment during the next belly laugh.
More Than Just a Bag: Why Support Matters
Imagine your bladder isn't much more than a muscular sac designed to stretch as it fills with urine produced by your kidneys. Now, picture that sac sitting somewhere in your lower belly. Without a dedicated anchoring system, what happens? Every step, cough, jump, or chuckle would send it bouncing around like a water balloon in a backpack. Leaks would be constant, not just occasional surprises. Positioning would be off, making complete emptying difficult and setting the stage for infections. It would be chaos!
Thankfully, our bodies are brilliantly engineered. The bladder doesn't just float freely. It’s meticulously suspended and cradled by a team of dedicated supporters – a combination of muscles, ligaments, and even its neighboring organs. Let’s pull back the curtain and meet these unsung heroes.
The Mighty Floor: Your Pelvic Diaphragm (The Hammock)
The absolute bedrock of bladder support comes from below. Think of your pelvic floor muscles as a dynamic, sling-like hammock stretching across the very bottom of your pelvis, from your tailbone at the back to your pubic bone at the front. This isn't one single muscle, but a complex team (including the levator ani and coccygeus muscles) working in concert.
How it Works: Your bladder sits directly on top of this muscular hammock. When these muscles are strong and toned, they provide a firm, supportive shelf. When you cough, laugh, sneeze, or lift something heavy, these muscles automatically contract and lift upwards, providing crucial counter-pressure against the downward force pushing on your bladder. It’s like having an internal security guard instantly bracing the door against a sudden push.
Real-World Connection: Ever heard of Kegels? Those exercises everyone (yes, everyone!) should be doing? They specifically target these pelvic floor muscles. Strengthening them is like reinforcing the foundation of your bladder’s house. Weak pelvic floor muscles are a primary culprit behind stress incontinence (leaking with exertion). Think about pregnancy and childbirth – huge strains on this supportive hammock, explaining why new moms often need focused rehab. Even chronic coughing (hello, smokers!), obesity, or just the natural weakening with age can challenge this vital support layer. What are the supports of the urinary bladder? The pelvic floor is arguably the MVP.
The Trusty Cables: Ligaments (The Guy Wires)
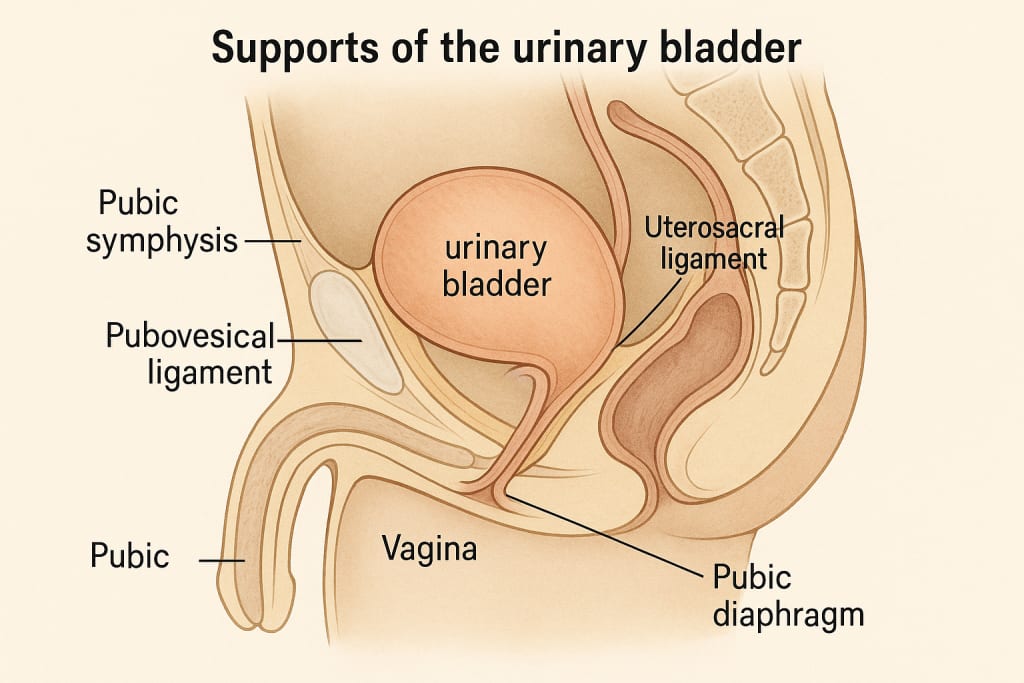
While the pelvic floor provides the primary shelf, ligaments act like strong, fibrous cables securing the bladder in its specific position within the pelvis, preventing excessive wobbling or sinking. Key players include:
The Pubovesical/Puboprostatic Ligaments: These attach the neck of the bladder (its lower, funnel-like end leading to the urethra) and, in men, the prostate gland, firmly to the back of the pubic bone. Picture sturdy straps tethering the front of the bladder down.
The Lateral Ligaments of the Bladder: Running sideways from the bladder walls into the surrounding pelvic wall connective tissue, these help stabilize the bladder's position laterally, stopping it from sliding too far side-to-side.
The Uterosacral Ligaments (in women): While primarily supporting the uterus and cervix, these ligaments also provide indirect, crucial posterior (back) support to the bladder base. Think of them as contributing to the overall structural integrity of the neighborhood.
The Rectovesical Fascia (in men): A tough sheet of connective tissue separating the bladder and prostate from the rectum in men. It provides significant posterior support.
How it Works: Ligaments are tough and relatively unyielding. They don't actively contract like muscles, but their inherent strength provides passive, constant anchorage. They define the bladder’s "parking spot" and prevent it from drifting too far out of position, especially during movements that might otherwise cause it to sag excessively downward.
Real-World Connection: Damage or stretching of these ligaments can happen during major pelvic surgery, significant trauma, or with severe, chronic prolapse. When these "guy wires" loosen, the bladder can descend lower than it should (a condition called cystocele in women), sometimes even bulging into the vagina. This descent puts extra strain on the urethra, often worsening leakage and making complete bladder emptying difficult. Understanding what are the supports of the urinary bladder highlights why pelvic organ prolapse involves a failure of multiple support systems, including these ligaments.
The Neighborly Nudge: Surrounding Organs and Fascia
The bladder doesn't exist in a vacuum. Its position is also subtly maintained by the organs packed tightly around it within the pelvis:
In Women: The uterus sits directly behind the bladder. A healthy, well-supported uterus contributes to keeping the bladder in its proper place. Conversely, a prolapsed uterus can drag the bladder down with it. The vagina also provides lateral support.
In Men: The prostate gland sits snugly below the bladder neck, acting like a supportive platform.
Fascia: Dense connective tissue sheets (endopelvic fascia) surround and connect the pelvic organs, acting like packing material and providing another layer of structural integration and support. Think of it as the internal webbing that helps hold everything together.
How it Works: It’s a team effort. The healthy shape and position of neighboring organs contribute to the overall stability of the pelvic environment. The fascia binds structures together, distributing forces and adding passive reinforcement.
Real-World Connection: A hysterectomy (removal of the uterus) requires surgeons to meticulously reattach supporting ligaments and fascia to the top of the vagina (the vaginal cuff) to prevent the bladder (and rectum) from subsequently sinking into the space left behind. It underscores how interconnected these support systems are.
The Internal Braces: The Bladder Neck and Urethra Themselves
Even the exit route plays a supporting role! The point where the bladder narrows into the urethra (the bladder neck) has a specific muscular structure designed to stay closed, acting as the primary internal seal. The urethra itself, especially in women where it’s shorter, runs through the pelvic floor muscles which wrap around it like a supportive sleeve (the urethral sphincter mechanism). This creates a secondary seal.
How it Works: While not "supports" in the positional sense like ligaments, the integrity of these closure mechanisms is vital for overall bladder control, which relies heavily on the positional stability provided by the other supports. If the bladder sags excessively (due to weak pelvic floor or ligaments), it can kink or distort the urethra, making these internal seals less effective.
Real-World Connection: Treatments for stress incontinence often focus on supporting the urethra (like mid-urethral slings) to compensate for weakened underlying structures, proving how intertwined positional support and internal closure are.
When the Supports Falter: The Leaky Reality
Understanding what are the supports of the urinary bladder suddenly makes sense of common problems:
Stress Incontinence: Weak pelvic floor muscles and/or stretched ligaments fail to counteract pressure (cough, sneeze, laugh, jump). Result? Leakage.
Urgency/Frequency: While often nerve-related, a significantly prolapsed bladder can irritate nerves or simply not hold as much, leading to feeling the need to go constantly.
Incomplete Emptying: A sagging bladder (cystocele) can create a "pouch" where urine pools, making it hard to fully void. This stagnant urine is a breeding ground for infections.
Pelvic Pressure/Pain: The sensation of something "falling out" or general heaviness in the pelvis is a classic sign of prolapse related to weakened supports.
Strengthening Your Silent Support Crew: What You Can Do
The fantastic news? You have direct influence over the most dynamic part of this support system: your pelvic floor muscles.
Master the Kegel (Properly!): This isn't just about squeezing randomly. It’s about isolating those specific muscles. Imagine trying to stop the flow of urine midstream (just to identify them, don’t do this regularly!) or clenching as if you're trying to prevent passing gas. You should feel a lift and squeeze inside your pelvis, not just your buttocks or thighs. Hold for 3-5 seconds, relax completely for 3-5 seconds. Aim for 10-15 reps, 3 times a day. Consistency is key!
Integrate Them: Once you’ve mastered the isolation, practice bracing your pelvic floor before you cough, sneeze, laugh, or lift anything heavy. This proactive bracing trains the reflex and provides real-time support.
Mind Your Mechanics: Avoid chronic straining during bowel movements (hello, fiber and water!). Lift heavy objects using your legs, not your back (and brace that pelvic floor!). Maintain a healthy weight – extra pounds put constant downward pressure on your pelvic floor.
Seek Expert Help: If you’re unsure about doing Kegels correctly, experiencing leaks, or feeling pelvic pressure, talk to your doctor or a pelvic floor physical therapist (PFPT). A PFPT is a specialist who can assess your specific muscles (yes, sometimes internally), tailor an exercise program, use biofeedback, and guide you through safe strengthening. Don't suffer in silence – help is available and incredibly effective.
A Final Thought: Honoring Your Hidden Architecture
What are the supports of the urinary bladder? It’s not a single answer, but a symphony – a muscular hammock, resilient ligaments, supportive neighbors, and intricate connective tissue, all working silently beneath your awareness. They are the reason you can run, dance, sneeze, and laugh without constant worry.
Understanding this hidden architecture isn't about memorizing anatomical terms; it's about appreciating the profound, often overlooked, engineering that allows for freedom and dignity in our daily lives. It empowers you to take proactive steps – through exercise, mindful movement, and seeking help when needed – to maintain this vital support system.
So, the next time you feel that familiar squeeze of laughter bubbling up, take a tiny, imperceptible moment. Feel the subtle lift and brace deep within your core – that’s your pelvic floor, your ligaments, your whole support crew, doing their job. It’s a silent thank you to the incredible, often unheralded, structures that hold us together, literally and figuratively, allowing us to move through the world with a little more confidence and a lot less worry. Invest in them, respect them, and they’ll support you for a lifetime.
About the Creator
Health Zone
Discover expert wellness tips, natural remedies, & nutrition hacks for busy lives. Science-backed advice for healthy living, glowing skin, & mindful habits. Join Health Zone—your shortcut to holistic vitality! 🌿






Comments
There are no comments for this story
Be the first to respond and start the conversation.