Women’s Gut Health: How Hormones Affect Digestion
Understanding the Powerful Link Between Female Hormones and Digestive Health—And How to Keep Your Gut in Balance Through Every Life Stage
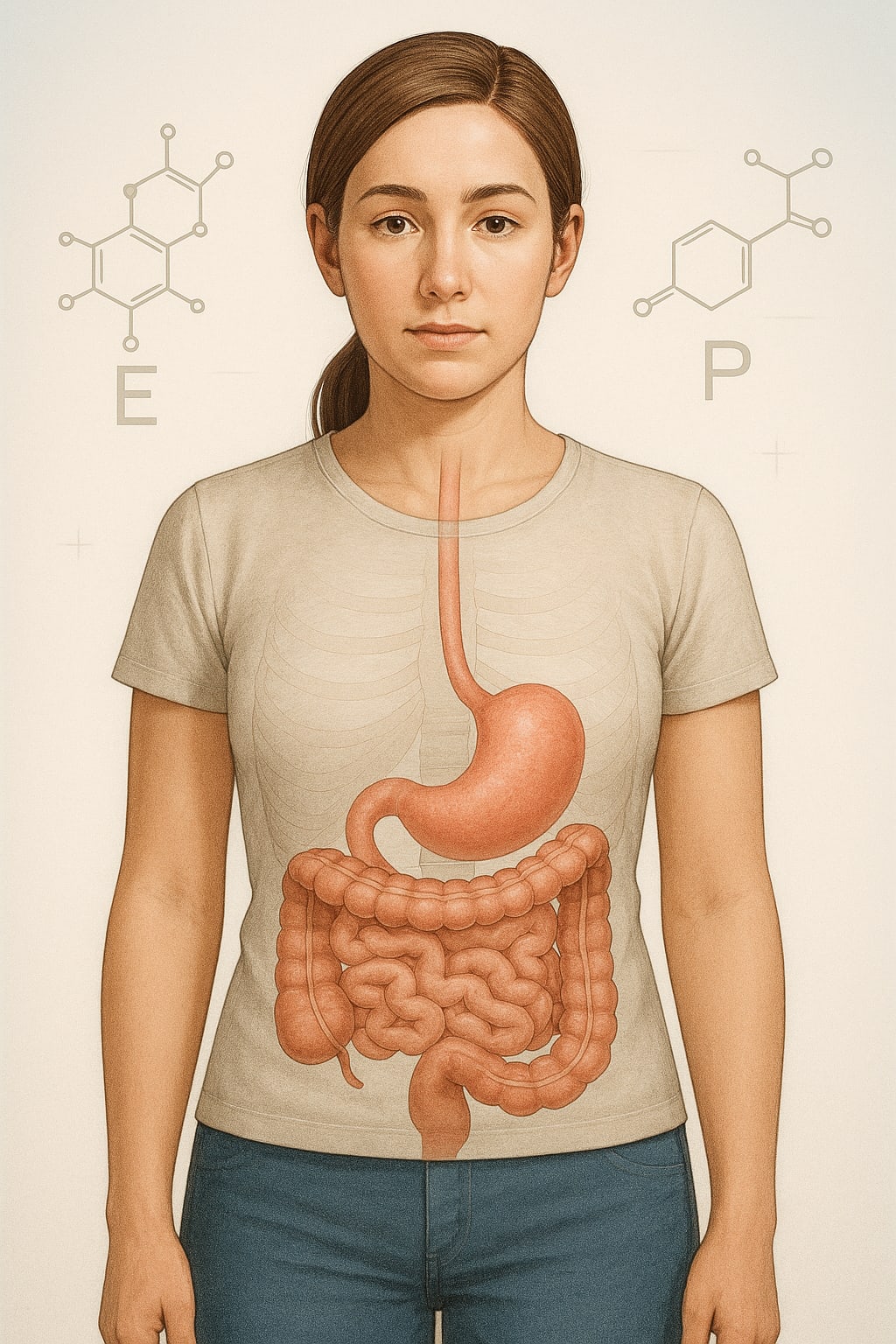
Gut health has become a hot topic in recent years, but for women, it’s not just about probiotics and fiber. Hormones—those chemical messengers that influence everything from mood to metabolism—also play a major role in how the digestive system works. If your digestion feels unpredictable at certain times of the month, or your gut symptoms flare during pregnancy or menopause, hormones could be the hidden trigger.
The Hormone–Gut Connection
The gut and the endocrine system are in constant communication. Hormones influence the speed of digestion, the sensitivity of the intestines, and even the types of bacteria living in the gut. When hormone levels rise or fall, the digestive system responds, sometimes in subtle ways and sometimes with noticeable discomfort.
Estrogen and progesterone, in particular, have a direct impact on gut motility—the speed at which food moves through the digestive tract. They also affect water retention, inflammation, and the balance of gut microbes. This is why digestive issues often appear alongside hormonal changes during the menstrual cycle, pregnancy, postpartum recovery, and menopause.
How Estrogen Affects Digestion
Estrogen generally promotes smooth muscle contraction in the intestines, helping food move efficiently. When estrogen is in balance, bowel movements tend to be regular, bloating is minimal, and digestion feels steady. But fluctuations can shift this harmony.
During the first half of the menstrual cycle, estrogen levels rise, which may make digestion feel more stable. However, just before menstruation, estrogen levels drop sharply. This decrease can contribute to constipation or bloating in some women, while others experience looser stools due to the combined effects of hormone changes and prostaglandins—chemicals released during menstruation that stimulate uterine and intestinal contractions.
Low estrogen, as seen in menopause, can slow gut motility and alter the balance of beneficial bacteria. This shift can lead to more frequent bloating, slower digestion, and changes in stool consistency.
The Role of Progesterone
Progesterone is known for its calming, slowing effects—not just on mood, but on digestion too. Higher progesterone levels, which occur in the second half of the menstrual cycle, relax the muscles of the digestive tract. This can cause food to move more slowly, leading to feelings of fullness, constipation, or increased bloating.
This same effect is amplified during pregnancy, when progesterone levels are significantly elevated. Many pregnant women experience constipation as a direct result of this hormonal influence, compounded by the physical pressure of the growing uterus.
The Gut Microbiome and Hormonal Balance
Inside the gut lives a vast community of bacteria, fungi, and other microorganisms collectively known as the microbiome. These microbes don’t just aid digestion—they also influence hormone metabolism.
Certain gut bacteria are responsible for breaking down estrogen in the body. If the microbiome becomes imbalanced (a condition called dysbiosis), estrogen may be reabsorbed instead of eliminated, leading to excess estrogen levels. This can trigger symptoms such as bloating, mood swings, or irregular cycles.
Hormonal fluctuations, in turn, can alter the microbiome’s diversity. For example, estrogen supports certain beneficial bacterial strains, while low estrogen can reduce them, creating an environment where less helpful microbes thrive.
Stress, Cortisol, and Digestion
Cortisol, the body’s main stress hormone, also interacts with digestion. Chronic stress raises cortisol levels, which can slow digestion, increase gut permeability, and cause shifts in the microbiome. For women already experiencing cyclical hormonal changes, ongoing stress can magnify symptoms like gas, cramping, and irregular bowel habits.
The combination of hormonal shifts and elevated cortisol often explains why gut symptoms are worse during emotionally or physically stressful periods.
Hormonal Milestones and Digestive Changes
Puberty
The surge in estrogen and progesterone during puberty can trigger digestive adjustments. Many young women notice changes in bowel patterns or increased sensitivity to certain foods as their bodies adapt to these new hormone levels.
Pregnancy
Progesterone slows digestion, while estrogen increases blood flow to the digestive tract. These changes can cause heartburn, constipation, and bloating, especially in later trimesters.
Postpartum
After childbirth, hormone levels drop dramatically. The gut may feel unsettled, and the microbiome may shift due to pregnancy, delivery, and postpartum stress.
Menopause
Declining estrogen affects gut motility and microbiome composition. Women may experience more bloating, constipation, or food sensitivities during this stage.
Supporting Gut Health Through Hormonal Changes
While you can’t stop hormonal fluctuations entirely, you can support your digestive system with targeted lifestyle strategies.
- Prioritize fiber from vegetables, fruits, legumes, and whole grains to keep bowel movements regular.
- Stay hydrated to prevent constipation and reduce bloating.
- Incorporate probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi to nourish a balanced microbiome.
- Limit processed foods that can inflame the gut and disrupt microbial diversity.
- Manage stress through mindfulness, deep breathing, or light physical activity to keep cortisol in check.
- Exercise regularly to stimulate digestion and improve overall hormone balance.
When to Seek Medical Advice
If you experience persistent bloating, abdominal pain, irregular bowel movements, or new digestive symptoms that coincide with hormonal changes, it’s worth discussing with a healthcare provider. They can assess whether hormonal shifts are the primary cause or if another underlying condition—such as irritable bowel syndrome, endometriosis, or thyroid imbalance—is contributing.
Bottom line: Women’s gut health is deeply connected to hormonal rhythms. Estrogen and progesterone shape digestion, while stress hormones and life-stage changes can intensify gut symptoms. By understanding these connections and making supportive lifestyle adjustments, you can help keep digestion steady through every hormonal shift.
About the Creator
Richard Bailey
I am currently working on expanding my writing topics and exploring different areas and topics of writing. I have a personal history with a very severe form of treatment-resistant major depressive disorder.






Comments
There are no comments for this story
Be the first to respond and start the conversation.