Ozempic: A Breakthrough in Diabetes Management and Weight Loss
A miracle diet drug

Ozempic is a medication approved by the FDA primarily for the management of type 2 diabetes. You may have heard its catchy jingle, “Oh, oh, oh Ozempic,” or seen headlines linking it to significant weight loss, often described as a “miracle diet drug.” While Ozempic was designed to assist individuals in managing their blood sugar levels, it has also shown remarkable effectiveness in promoting weight loss.
Patients have reported notable weight reductions as a side effect. One user shared, “My doctor mentioned this was mainly for blood sugar management, but as a side effect, I found I was losing weight.” After noticing a ten-pound drop in just the first month, many have begun to see the potential for this drug to transform our approach to weight management.
According to recent data from the National Institutes of Health, approximately 42% of adults in the U.S. are classified as obese. The CDC lists several health risks associated with obesity, including heart disease, stroke, and type 2 diabetes—conditions that rank among the leading causes of premature death globally. While not all individuals with type 2 diabetes are classified as obese, there is a strong correlation between the two conditions. In fact, weight loss is often recommended as a key strategy for managing type 2 diabetes, as even modest reductions in weight can significantly aid blood sugar control.
I spoke with Mila Clarke, a 33-year-old diagnosed with latent autoimmune diabetes in adults, who runs a YouTube channel called Hangry Woman, where she shares her journey living healthily with diabetes. Mila emphasized the struggle of managing both diabetes and obesity, noting, “It's incredibly challenging.” She has also shared her experience with Ozempic, stating that despite her efforts with diet and exercise, losing weight remained difficult.
Historically, weight loss medications have faced criticism due to dangerous side effects, leading to many being withdrawn from the market. Metabolic and bariatric surgery offers effective weight loss results but requires significant lifestyle changes that can be tough to maintain. With the advent of newer diabetes medications like Ozempic, however, there is hope for a safer and more effective weight management solution, rooted in the body’s natural hormones.
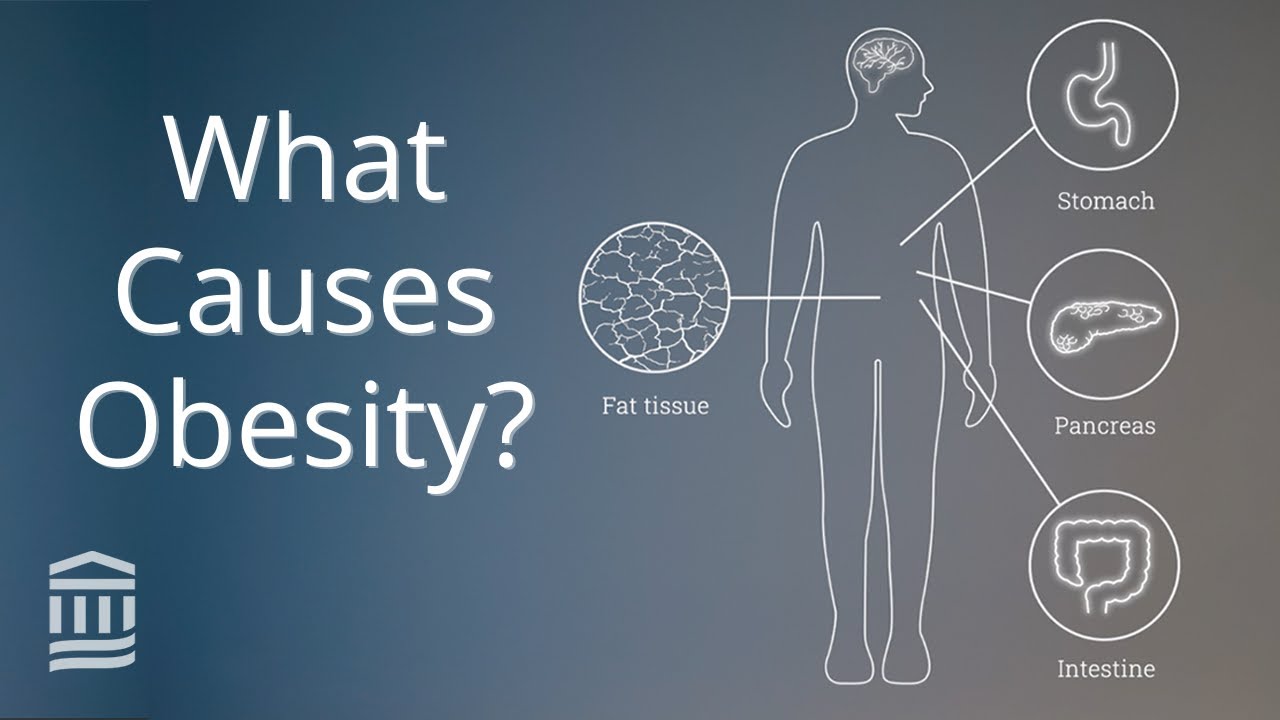
One such hormone is GLP-1 (glucagon-like peptide-1), which plays a crucial role in appetite regulation. When we eat, our bodies release GLP-1 from the intestine, signaling fullness. This is where semaglutide, the generic name for Ozempic, comes in: it is designed to mimic GLP-1's effects.
GLP-1 receptors are present throughout the body and serve various functions. In the pancreas, they stimulate insulin production (which lowers blood sugar levels) and suppress glucagon (which raises blood sugar levels). This is particularly vital for individuals with type 2 diabetes, who often face insulin resistance. By enhancing the body’s natural insulin, semaglutide can improve blood sugar management.
Additionally, GLP-1 receptors in the stomach slow gastric emptying, allowing food to remain longer in the digestive tract, which contributes to prolonged feelings of fullness and helps mitigate blood sugar spikes. Notably, GLP-1 receptors in the brain—especially in the hypothalamus—help suppress hunger cravings, making it easier to control intake.
Clinical trials of semaglutide have shown significant results, with participants experiencing an average weight loss of about 15% when combined with dietary adjustments and exercise, compared to a mere 2% weight loss in a placebo group. This level of effectiveness rivals that of metabolic and bariatric surgery, demonstrating the potential of this medication. One patient remarked, “The fact that I was able to take a once-weekly injection and see the pounds drop off was wild to me.”
While Ozempic has its side effects—most commonly nausea and gastrointestinal issues like diarrhea—many users, including Mila, find the benefits outweigh the drawbacks. After initially discontinuing Ozempic due to heart palpitations, she returned to the medication and reported improved blood sugar levels, weight loss, and increased activity in her life.
Since its introduction in late 2017, prescriptions for semaglutide have surged. In 2021, the FDA approved a higher dose of semaglutide specifically for weight management under the brand name Wegovy. This shift in focus has led to increased interest in the drug, but it has also raised concerns that its importance for diabetes management may be overlooked in the narrative surrounding its weight loss benefits.
Mila points out the challenges posed by the growing demand for these medications: “There are two groups of people—those who need this drug for health reasons and those who see it as an easy weight loss solution.”
To address this demand, Mounjaro, another medication designed for type 2 diabetes, is being expedited for approval for weight management. With Ozempic’s rising popularity, medications like it are likely to become more widely prescribed for weight loss.
It’s important to note that using Ozempic is not a simple fix for obesity or diabetes. Effective management still requires a commitment to a healthy lifestyle. However, the emergence of such innovative treatments brings hope for those battling these conditions.
As Mila summarizes, “It’s exciting to see innovations that can make our lives easier, reduce diabetes burnout, and help us focus less on managing the condition.”




Comments
There are no comments for this story
Be the first to respond and start the conversation.