Duodenal Ulcer - Causes, Symptoms, Diagnosis and Treatment
Peptic ulcer. Symptoms. Diagnostics. What to do with the diagnosis of peptic ulcer of the 12p. intestine. Conservative treatment and operations.
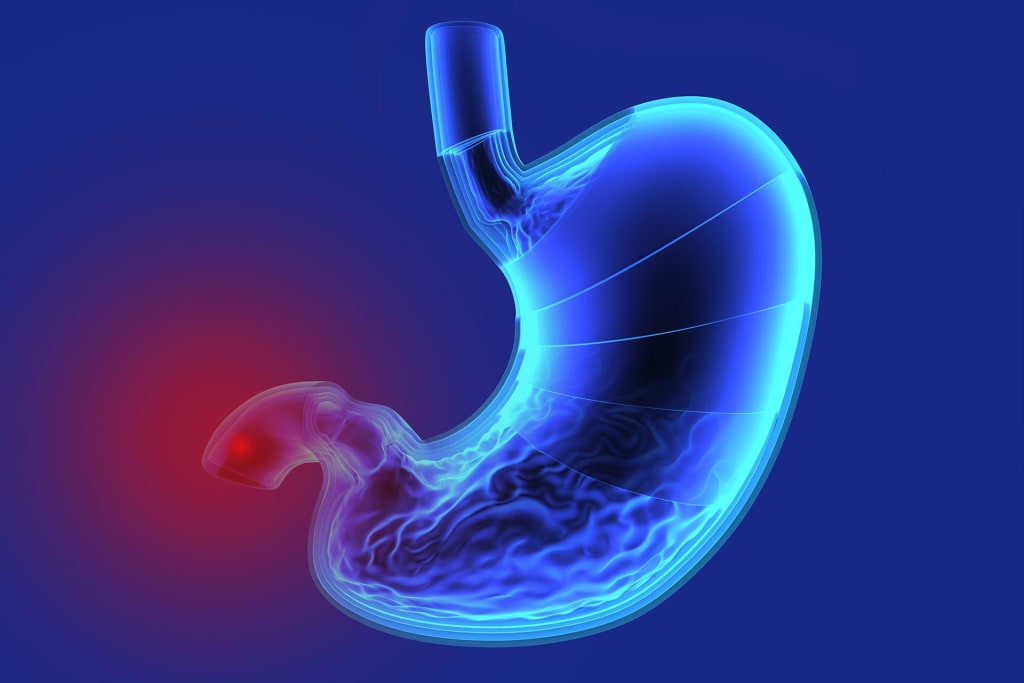
Ulcer of the duodenum is a disease of the duodenum of a chronic recurrent nature, accompanied by the formation of a defect in its mucous membrane and the tissues located under it. It is manifested by severe pain in the left epigastric region, occurring 3-4 hours after eating, attacks of "hungry" and "night" pains, heartburn, belching acid, often vomiting. The most serious complications are bleeding, perforation of the ulcer and its malignant degeneration. Diagnosis includes gastroscopy with biopsy, stomach radiography, urease breath test. The main directions of treatment are eradication of helicobacter infection, antacid and gastroprotective therapy.
General information
Duodenal ulcer is a chronic disease characterized by the occurrence of ulcerative defects of the duodenal mucosa. It proceeds for a long time, alternating periods of remission with exacerbations. Unlike erosive mucosal lesions, ulcers are deeper defects that penetrate into the submucosal layer of the intestinal wall. Duodenal ulcer occurs in 5-15% of the population (statistics vary depending on the region of residence), more often occurs in men. Duodenal ulcer is 4 times more common than stomach ulcer.
Reasons
The modern theory of the development of peptic ulcer disease considers the key factor in its occurrence to be an infectious lesion of the stomach and duodenum by Helicobacter Pylori bacteria. This bacterial culture is sown during bacteriological examination of gastric contents in 95% of patients with duodenal ulcer and in 87% of patients suffering from gastric ulcer.
However, infection with helicobacteria does not always lead to the development of the disease, in most cases there is an asymptomatic carrier. Factors contributing to the development of duodenal ulcer:
- alimentary disorders - improper, irregular diet;
- frequent stress;
- increased secretion of gastric juice and decreased activity of gastroprotective factors (gastric mucoproteins and bicarbonates);
- smoking, especially on an empty stomach;
- prolonged use of medications that have an ulcerogenic (ulcerative) effect (most often these are drugs of the group of nonsteroidal anti-inflammatory drugs - analgin, aspirin, diclofenac, etc.);
- gastrin-producing tumor (gastrinoma).
Duodenal ulcers resulting from taking medications or concomitant gastrinoma are symptomatic and are not included in the concept of peptic ulcer disease.
Classification
Peptic ulcer disease differs in localization:
- Gastric ulcer (cardia, subcardial region, stomach body);
- peptic postresection ulcer of the pyloric canal (anterior, posterior wall, small or large curvature);
- duodenal ulcer (bulbous and postbulbar);
- ulcer of unspecified localization.
According to the clinical form, acute (newly identified) and chronic peptic ulcer disease are distinguished. According to the phase, periods of remission, exacerbation (relapse) and incomplete remission or fading exacerbation are distinguished. Peptic ulcer disease can occur:
- latently (without a pronounced clinic),
- easily (with rare relapses),
- moderate severity (1-2 exacerbations during the year)
- is severe (with regular exacerbations up to 3 or more times a year).
The duodenal ulcer itself differs:
1 According to the morphological picture: acute or chronic ulcer.
2 In size: small (up to half a centimeter), medium (up to a centimeter), large (from one to three centimeters) and giant (more than three centimeters) in size.
Stages of ulcer development: active, scarring, "red" scar and "white" scar. With concomitant functional disorders of the gastroduodenal system, their nature is also noted: violations of motor, evacuation or secretory function.
Symptoms
In children and the elderly, the course of peptic ulcer disease is sometimes almost asymptomatic or with minor manifestations. This course is fraught with the development of severe complications, such as perforation of the wall of the duodenum with subsequent peritonitis, latent bleeding and anemia. A typical clinical picture of duodenal ulcer is a characteristic pain syndrome.
The pain is most often moderate, dull. The severity of the pain depends on the severity of the disease. Localization is usually from the epigastrium, under the sternum. Sometimes the pain can be spread in the upper half of the abdomen. It often occurs at night (1-2 hours) and after prolonged periods without eating, when the stomach is empty. After taking food, milk, antacid drugs, relief comes. But most often the pain resumes after the evacuation of the stomach contents.
The pain may occur several times a day for several days (weeks), after which it will pass on its own. However, over time, without proper therapy, relapses become more frequent, and the intensity of the pain syndrome increases. The seasonality of relapses is characteristic: exacerbations occur more often in spring and autumn.
Complications
The main complications of duodenal ulcers are penetration, perforation, bleeding and narrowing of the intestinal lumen. Ulcerative bleeding occurs when the pathological process affects the vessels of the gastric wall. Bleeding may be hidden and manifest only by increasing anemia, or it may be pronounced, blood may be detected in vomiting and manifest during defecation (black or with bloody streaks of feces). In some cases, it is possible to stop bleeding during an endoscopic examination, when the source of bleeding can sometimes be cauterized. If the ulcer is deep and the bleeding is abundant, surgical treatment is prescribed, in other cases they are treated conservatively, correcting iron deficiency. With ulcerative bleeding, patients are prescribed strict hunger, parenteral nutrition.
Perforation of the duodenal ulcer (usually the anterior wall) leads to the penetration of its contents into the abdominal cavity and inflammation of the peritoneum - peritonitis. When the intestinal wall is pierced, there is usually a sharp cutting-stabbing pain in the epigastrium, which quickly becomes diffuse, increases with a change of body position, deep breathing. The symptoms of irritation of the peritoneum (Shchetkin-Blumberg) are determined – when pressing on the abdominal wall, and then abruptly releasing the pain increases. Peritonitis is accompanied by hyperthermia. This is an emergency condition that, without proper medical care, leads to the development of shock and death. Perforation of an ulcer is an indication for urgent surgical intervention.
Ulcer penetration is a deep defect affecting the intestinal wall with penetration into adjacent organs (liver or pancreas). It is manifested by intense pain of a stabbing nature, which can be localized in the right or left hypochondrium, radiate into the back, depending on the location of the penetration. When the position changes, the pain increases. Treatment, depending on the severity, is conservative, in the absence of a result, it is operative.
Duodenal stenosis occurs with pronounced swelling of the ulcerated mucosa or scar formation. With narrowing of the lumen, an obstruction (complete or partial) of the duodenum occurs. It is often characterized by repeated vomiting. In the vomit, the food taken long before the attack is determined. Also, the symptoms are characterized by heaviness in the stomach (overflow), lack of stool, bloating. Regular vomiting contributes to weight loss and metabolic disorders associated with nutritional deficiencies. Most often, conservative treatment leads to a decrease in swelling of the walls and expansion of the lumen, but with severe scarring changes, stenosis can become permanent and require surgical intervention.
Diagnostics
The survey reveals the nature of the pain syndrome, its connection with meals, the seasonality of seizures, concomitant symptoms. The most informative diagnostic methods are:
- Gastroscopy. Endoscopic examination of the mucous membranes of the stomach and duodenum gives detailed information about the localization of the ulcer and its morphological features, reveals bleeding and scarring. With FGDS, it is possible to perform a biopsy of the stomach and DPC tissues for histological examination.
- Stomach X-ray. During an X-ray examination with a contrast agent, duodenal ulcer manifests itself as a wall defect (the barium mixture penetrates the ulcer and this can be seen on the X-ray), intestinal stenosis, perforation and penetration of ulcers are detected.
- Detection of helicobacter infection. To detect infection with helicobacteria, PCR diagnostics and a urease respiratory test are used.
- Laboratory methods. Laboratory blood tests can detect signs of anemia, which indicates the presence of internal bleeding. Fecal masses are also examined for hidden blood. During duodenal probing, data on the state of the WPC environment are obtained.
Treatment of duodenal ulcer
Treatment of duodenal ulcers is carried out strictly according to the prescription of a gastroenterologist, self-medication is unacceptable due to the fact that self-administration of drugs that help to get rid of pain leads to symptoms and latent development of the disease, which threatens complications. Drug therapy of duodenal ulcer disease includes measures for the eradication of Helicobacter and the healing of ulcerative defects (which is facilitated by a decrease in the acidity of gastric juice).
- To suppress helicobacter infection, broad-spectrum antibiotics (metronidazole, amoxicillin, clarithromycin) are used, antibiotic therapy is carried out for 10-14 days.
- To reduce the secretory activity of the stomach, the optimal drugs are proton pump inhibitors - omeprazole, esomeprazole, lanzoprazole, rabeprazole. For the same purpose, agents that block H2-histamine receptors of the gastric mucosa are used: ranitidine, famotidine. Antacids are used as agents that reduce the acidity of gastric contents.
- Gel antacids with anesthetics are also effective as symptomatic drugs - they relieve pain by enveloping the intestinal wall.
- To protect the mucosa, gastroprotective agents are used: sucralfate, bismuth preparations, misoprostol.
If conservative treatment is ineffective or if dangerous complications develop, surgical treatment is resorted to. The operation consists in excision or suturing of a duodenal ulcer. If necessary, vagotomy is performed to reduce secretion.
Prognosis and prevention
Measures to prevent the development of duodenal ulcer:
- timely detection and treatment of helicobacter infection;
- normalization of the regime and nature of nutrition;
- quitting smoking and alcohol abuse;
- monitoring of medications taken;
- harmonious psychological environment, avoidance of stressful situations.
Uncomplicated peptic ulcer disease, with proper treatment and compliance with dietary and lifestyle recommendations, has a favorable prognosis, with high-quality eradication - ulcer healing and healing. The development of complications in peptic ulcer disease aggravates the course and can lead to life-threatening conditions.
About the Creator
Artur Kh.
Writer, doctor and businessman. I blog about self-development, personal growth, health and new ways of making money.






Comments
There are no comments for this story
Be the first to respond and start the conversation.