Deep Vein Thrombosis (DVT): Causes, Risks, and Prevention
Understanding Deep Vein Thrombosis: Causes, Risks, and How to Prevent Life-Threatening Blood Clots."
Introduction
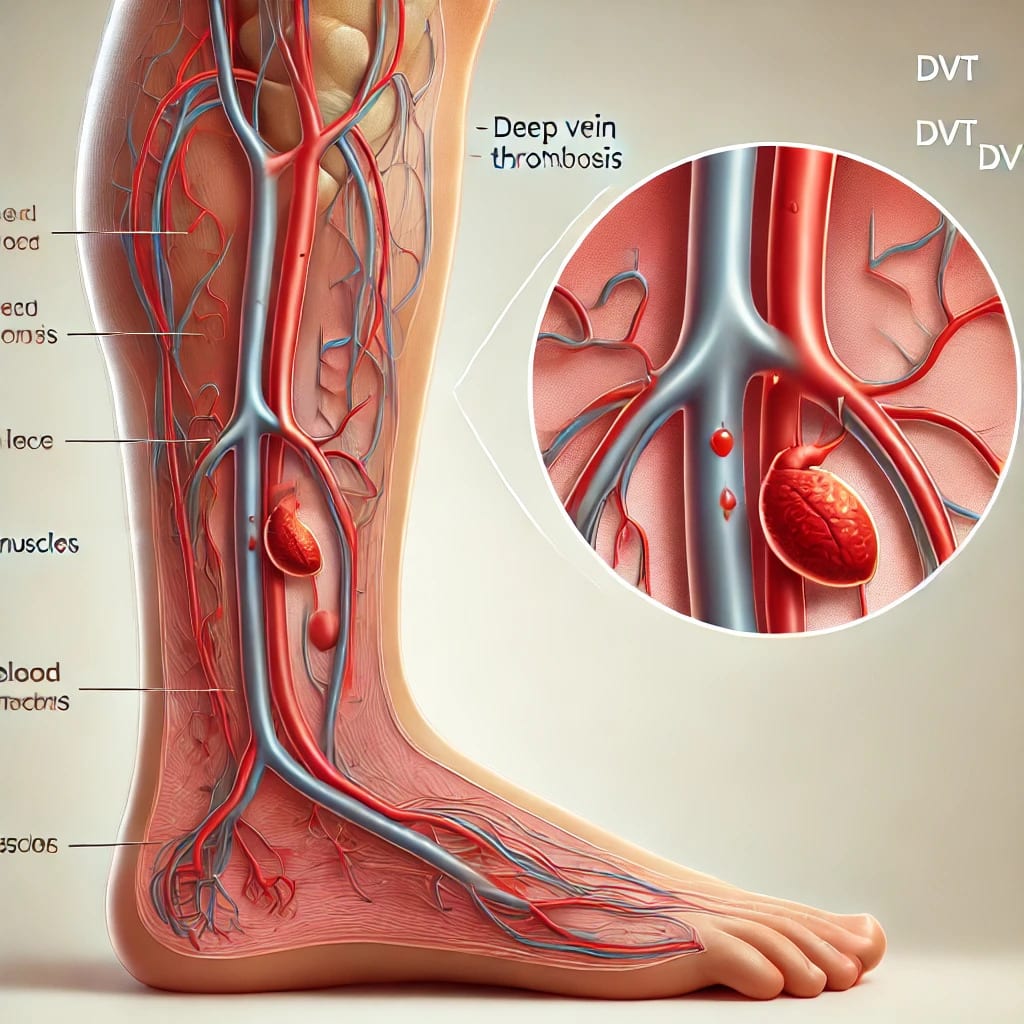
Deep Vein Thrombosis (DVT) is a serious medical condition that occurs when a blood clot forms in a deep vein, usually in the legs. While it may not always cause immediate symptoms, DVT can lead to life-threatening complications if the clot dislodges and travels to the lungs, resulting in a pulmonary embolism (PE). Understanding the causes, symptoms, risk factors, and prevention methods is crucial for maintaining vascular health and preventing severe consequences.
In this article, we will explore everything you need to know about DVT, including its causes, symptoms, complications, treatment options, and how you can reduce your risk.
What Is Deep Vein Thrombosis?
Deep Vein Thrombosis is a condition where a blood clot (thrombus) forms in a deep vein, most commonly in the lower legs, thighs, or pelvis. The clot partially or completely blocks blood flow, which can cause swelling, pain, and other complications.
The most dangerous aspect of DVT is the risk of embolization—when the clot breaks loose and travels through the bloodstream. If it reaches the lungs, it can cause a pulmonary embolism, a life-threatening condition that requires immediate medical attention.
Causes of Deep Vein Thrombosis
DVT typically develops due to three main factors, known as Virchow’s Triad:
Slow or Stagnant Blood Flow
Long periods of inactivity (e.g., sitting for hours during travel)
Bed rest after surgery or injury
Paralysis or immobility due to medical conditions
Increased Blood Clotting Tendency
Genetic clotting disorders (e.g., Factor V Leiden mutation)
Cancer and chemotherapy treatments
Hormonal changes (e.g., pregnancy, birth control pills, hormone replacement therapy)
Damage to Blood Vessel Walls
Surgery or trauma to veins
Catheter use in veins (such as central venous catheters)
Chronic inflammation due to diseases like autoimmune disorders
Symptoms of Deep Vein Thrombosis
DVT symptoms can vary depending on the size and location of the clot. Some individuals may experience no symptoms at all, while others might notice the following:
Swelling in the affected leg, often occurring suddenly
Pain or tenderness in the leg, usually in the calf or thigh
Skin discoloration, appearing red or bluish
Warmth in the affected area
Enlarged veins that become visible and tender
If you experience these symptoms, particularly after long periods of immobility, it is essential to seek medical attention immediately.
Complications of DVT: Pulmonary Embolism (PE)
One of the most severe complications of DVT is pulmonary embolism (PE). This occurs when a clot breaks free from the vein and travels to the lungs, blocking blood flow.
Signs of Pulmonary Embolism
A pulmonary embolism is a medical emergency and can cause:
Sudden shortness of breath
Chest pain or discomfort that worsens with deep breathing
Rapid heart rate
Coughing up blood
Feeling faint or dizzy
If you suspect a PE, call emergency services immediately, as it can be fatal if left untreated.
Who Is at Risk for DVT?
Several risk factors can increase the likelihood of developing DVT:
Prolonged Immobility
Long flights or car rides (sitting for more than 4-6 hours)
Hospitalization and bed rest
Paralysis or sedentary lifestyle
Medical Conditions
Cancer (especially blood-related cancers like leukemia)
Heart failure
Obesity
Inflammatory diseases (e.g., lupus, rheumatoid arthritis)
Pregnancy and Hormonal Changes
Pregnancy increases pressure on veins in the pelvis and legs
Oral contraceptives and hormone replacement therapy can increase clotting risk
Genetic Blood Disorders
Factor V Leiden mutation
Prothrombin gene mutation
Antithrombin III, protein C, or protein S deficiency
Surgery or Injury
Major surgeries, especially orthopedic procedures (hip/knee replacements)
Spinal cord injuries that limit movement
Smoking
Smoking damages blood vessels and increases clotting risk
Age and Family History
Risk increases after age 60
Having a family history of DVT raises the likelihood of developing clots
Diagnosis: How Is DVT Detected?
Doctors use several diagnostic methods to confirm DVT, including:
1. Ultrasound (Doppler Ultrasound)
The most common and non-invasive test
Uses sound waves to detect blood clots in veins
2. D-Dimer Test
A blood test that measures clot breakdown products
High levels may indicate the presence of a blood clot
3. Venography
A contrast dye is injected into veins to provide X-ray imaging
Less commonly used but highly effective
4. MRI or CT Scans
Used in cases where ultrasound is inconclusive
Helps detect clots in deeper veins
Treatment Options for DVT
1. Blood Thinners (Anticoagulants)
Common medications include Warfarin, Heparin, Apixaban (Eliquis), and Rivaroxaban (Xarelto)
Prevents further clot growth and reduces risk of embolization
2. Thrombolytic Therapy ("Clot Busters")
Used in severe cases to dissolve large clots
Typically administered in emergency situations
3. Compression Stockings
Prevent swelling and improve circulation in the affected leg
4. Inferior Vena Cava (IVC) Filter
A small device inserted into the vena cava (largest vein) to catch clots before they reach the lungs
Used when blood thinners are not an option
Preventing DVT: Steps You Can Take
1. Stay Active
Avoid sitting for extended periods
Stand up and walk every 1-2 hours during long trips
2. Wear Compression Stockings
Especially helpful for those with circulatory issues or after surgery
3. Stay Hydrated
Dehydration thickens blood, increasing clot risk
4. Maintain a Healthy Weight
Obesity is a major risk factor for DVT
5. Avoid Smoking and Limit Alcohol
Both affect blood flow and increase clotting risks
6. Talk to Your Doctor if You’re at Risk
If you have a family history of DVT, discuss preventative medications with your doctor
Conclusion
Deep Vein Thrombosis is a serious condition that can lead to life-threatening complications like pulmonary embolism. However, with early detection, proper treatment, and preventive measures, the risk of severe outcomes can be significantly reduced.
By staying active, managing risk factors, and seeking medical attention for any symptoms, individuals can protect themselves from the dangers of blood clots and DVT-related complications.






Comments
There are no comments for this story
Be the first to respond and start the conversation.