Understanding the Link Between Oral Contraceptive Pills and Deep Vein Thrombosis
Balancing Benefits and Risks

Oral contraceptive pills (OCPs) are among the most widely used methods of birth control worldwide. They provide an effective means of preventing pregnancy and can also offer other health benefits, like regulating menstrual cycles and reducing the symptoms of certain hormonal disorders. However, their use is not without risks. One serious concern is the potential increased risk of deep vein thrombosis (DVT), a condition that can lead to significant and sometimes fatal complications.
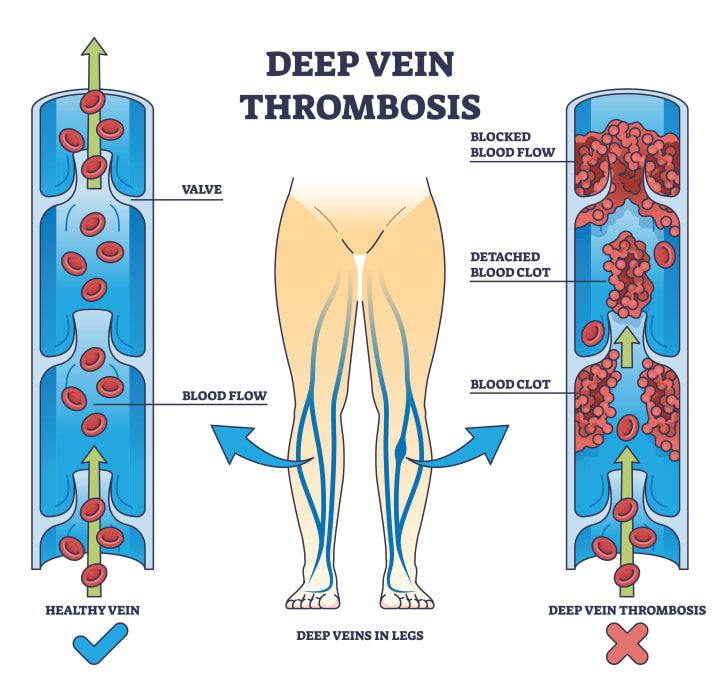
What is Deep Vein Thrombosis?
Deep vein thrombosis occurs when a blood clot forms in a deep vein, usually in the legs. This clot can cause pain, swelling, and redness in the affected limb. More alarmingly, if the clot breaks loose, it can travel to the lungs, creating a pulmonary embolism, which can be life-threatening.
How Oral Contraceptives Can Increase DVT Risk
The link between oral contraceptives and DVT is primarily due to the hormones contained in these pills, which can affect the body’s clotting system. Estrogen, in particular, is known to increase the production of clotting factors, which can make the blood more prone to clotting. This is a natural mechanism intended to prevent excessive bleeding during childbirth, but in the context of OCPs, it can enhance the risk of clot formation inappropriately.
Differences in Oral Contraceptive Formulations
Not all oral contraceptives carry the same risk. The type and amount of estrogen, the type of progestin, and how the pill is dosed can all affect DVT risk:
Estrogen levels and types: Pills with higher doses of estrogen or certain types of synthetic estrogen might have a higher risk associated with them.
Progestin-only pills: Also known as the "mini-pill," these are believed to carry a lower risk of DVT compared to those containing both estrogen and progestin.
Third-generation progestins: Some studies suggest that pills containing newer forms of progestin, like desogestrel and gestodene, might have a higher risk of DVT than those with older progestins like levonorgestrel.
Recent scientific studies, including those published in major journals like The Lancet and Journal of Thrombosis and Haemostasis, have helped clarify these differences, though results can vary and ongoing research continues to refine our understanding.
Additional Risk Factors
When considering OCPs, it's important to consider personal and lifestyle factors that can further influence DVT risk:
Age: Risk increases with age, especially over 35.
Smoking: Tobacco use significantly increases DVT risk, especially when combined with OCP use.
Obesity: Higher body weight is associated with an increased risk of blood clots.
Genetic factors: Some genetic mutations can increase clotting risk independently of OCP use.
Preventative Measures
There are several ways to mitigate the risk of DVT when using oral contraceptives:
Medical Assessment: Before starting OCPs, discuss your medical history and any potential risk factors with a healthcare provider.
Regular Monitoring: Once on OCPs, regular follow-ups can help catch any potential issues early.
Lifestyle Changes: Maintaining a healthy weight, quitting smoking, and staying active can all help reduce DVT risk.
Alternatives to Oral Contraceptives
For those concerned about the risks associated with OCPs, there are alternatives:
Intrauterine devices (IUDs): Both hormonal and copper IUDs are highly effective and do not carry the same risk of DVT.
Barrier methods: Condoms, diaphragms, and other barrier methods provide contraception without affecting the body’s hormonal balance.
Natural family planning: Methods based on tracking fertility can be effective if used consistently and correctly.
FAQs
Q: Can I use OCPs if I have a family history of DVT?
A: It's essential to discuss family medical history with your healthcare provider, as they may recommend a safer alternative based on your specific circumstances.
Q: Are there any signs I should watch for that might indicate a DVT?
A: Yes, symptoms like unexplained swelling, pain, and redness in one leg, especially if accompanied by shortness of breath, warrant immediate medical attention.
Q: How often should I see my doctor if I'm taking OCPs?
A: Annual check-ups are standard, but more frequent visits may be necessary if you have additional risk factors for DVT.
Understanding these factors and maintaining open communication with healthcare providers are key steps in managing health effectively while using oral contraceptives.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.