Understanding Diabetic Foot Ulcer Grading with Realistic Simulation Models
Practical Insights into Diabetic Foot Care Training Using Ultrassist Foot Ulcer Simulators
"When I first started my clinical rotations as a nursing student, I vividly remember my first encounter with a patient suffering from a diabetic foot ulcer. I felt a mix of curiosity and apprehension - how do I assess the severity without causing discomfort? How do I ensure that my interventions are both safe and effective? At the time, I had minimal hands-on practice, and observing patients in real life was intimidating. That's when I realized the profound value of simulation-based learning. Using a realistic diabetic foot model not only allowed me to practice safely but also helped me understand the subtle differences between ulcer grades, preparing me to deliver more confident and competent care."
Why Diabetic Foot Care Training is Critical
Diabetic foot ulcers are among the most common and serious complications for individuals with diabetes. Improper assessment or delayed intervention can lead to infections, hospitalization, and even amputation. According to the International Diabetes Federation, nearly 15% of diabetic patients develop foot ulcers during their lifetime. This statistic underscores the need for healthcare professionals to gain accurate, hands-on training in ulcer assessment and management.
However, traditional classroom instruction and textbook diagrams often fall short in conveying the tactile and visual cues that are essential for accurate grading. This is where realistic simulation models make a remarkable difference.
The Role of Simulation Models in Ulcer Grading
High-fidelity diabetic foot models replicate real-life foot anatomy, including skin texture, bone structure, and various ulcer stages. These models allow learners to:
- Identify subtle differences in wound depth and tissue involvement.
- Recognize signs of infection, necrosis, or callus formation.
- Practice safe cleaning, dressing, and pressure relief techniques.
- Understand the progression from Grade 1 superficial ulcers to Grade 5 severe, deep-tissue involvement.
By practicing on these models, students and clinicians can gain the confidence to make precise assessments in real clinical scenarios without putting patients at risk.
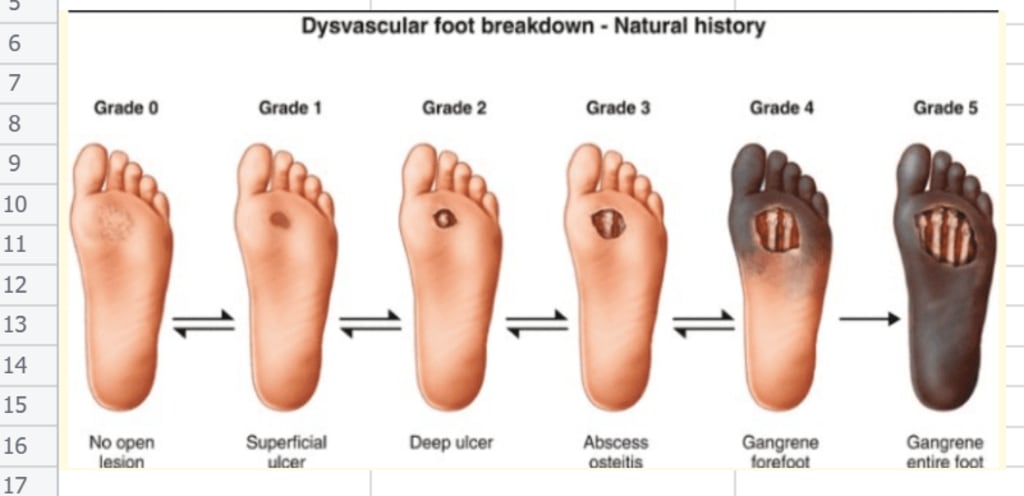
Understanding the 5 Ulcer Grades

Grade 1 (Superficial Ulcer): Confined to the skin, minimal tissue involvement. Often presents with redness or minor skin breakdown. Simulation models provide realistic tactile feedback to recognize early-stage lesions.
Grade 2 (Partial-Thickness Ulcer): Extends into subcutaneous tissue but not muscle or bone. Learners can practice wound cleaning and dressing changes safely using models that mimic tissue resistance.
Grade 3 (Full-Thickness Ulcer): Involves deeper tissue, possibly exposing bone or tendon. Realistic models help clinicians anticipate potential complications and refine their dressing and debridement techniques.
Grade 4 (Localized Gangrene): Tissue necrosis is evident, often limited to a portion of the forefoot or toes. Simulation models allow learners to study these severe scenarios without the risk of infection.
Grade 5 (Extensive Foot Gangrene): Involves widespread tissue necrosis and potential bone involvement. Handling such advanced stages on a model provides critical insight into surgical considerations and multidisciplinary care planning.
Advantages of Diabetic Foot Care Models
A Diabetic Foot Care Model – Grade 1-5 Foot Ulcer Simulation designed for high-fidelity clinical training. The advantages include:
- Realistic Anatomy: Mimics actual foot structure with varying ulcer grades.
- Tactile Feedback: Simulates tissue texture and resistance for accurate wound assessment.
- Safe Learning Environment: Allows repeated practice without patient risk.
- Comprehensive Grading Practice: Covers all five ulcer grades, from superficial to severe.

This model is an indispensable tool for nursing students, podiatrists, and healthcare educators aiming to enhance training outcomes.
Such a diabetic foot grading model, you can explore from Ultrassist, Nasco Healthcare, etc.
Integrating Simulation Models into Clinical Training
Using simulation models in a structured curriculum ensures that learners:
- Develop consistent assessment skills.
- Recognize early warning signs of foot ulcer progression.
- Gain confidence in implementing preventive care and dressing protocols.
- Improve decision-making for referrals and advanced interventions.
Combining theoretical knowledge with hands-on simulation practice bridges the gap between classroom learning and real-world clinical competence.
Conclusion
Realistic diabetic foot models are revolutionizing diabetic care education. They provide a safe, interactive, and effective platform for students and clinicians to practice ulcer grading, wound care, and preventive strategies. By incorporating Diabetic Foot Care Model into your training program, educators can ensure learners gain the practical experience necessary to improve patient outcomes and reduce the risks associated with diabetic foot complications.
Simulation-based learning is no longer optional; it's a vital component of modern healthcare education, empowering learners to act with skill, confidence, and compassion.
About the Creator
Ultrassist
We're Ultrassist, creators of realistic medical training models for nursing, EMS, and trauma care. Our blog offers tips, tutorials, and insights to support hands-on learning. Visit ultrassist.com for more.






Comments
There are no comments for this story
Be the first to respond and start the conversation.