Simple Lumber Radiculopathy, Simple Sciatica
Breaking down what lumbar radiculopathy truly is

“Lumbar radiculopathy.”
When first presented with the medical terminology for this injury, one would hastily assume that their leg would be impaired for life with treatments applied to no avail. Fortunately, a majority of the stress may be relieved when told that lumbar radiculopathy is synonymous with sciatica - it’s the same condition!
Sciatica is the common name for an unfortunately common injury - it occurs in approximately 40% of people in the United States (Berg, 2024).
Why not just use the word “sciatica”?
My curiosity threw me into a hole of web surfing as I hoped to uncover the power of calling sciatica “lumbar radiculopathy”. After various discoveries, I unexpectedly gained a strength of respect for the name - it’s beautiful, expressive, and purposeful.
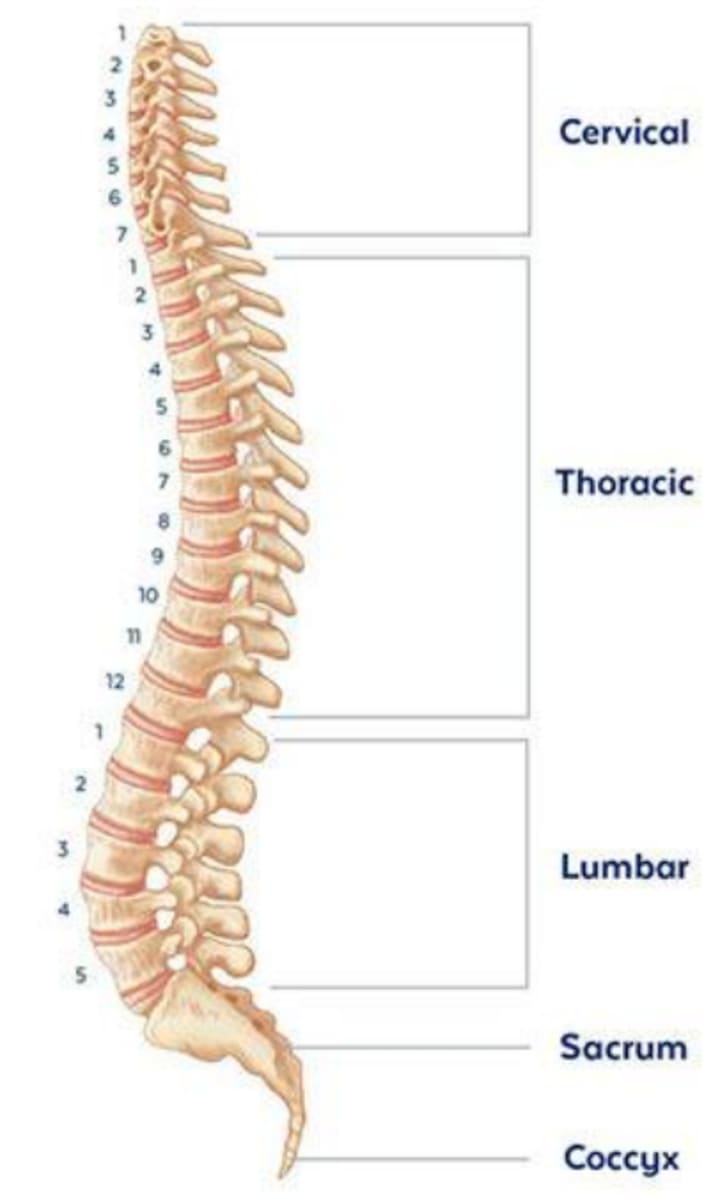
The spine, the pillar-like support found in our back, can be further broken down into the cervical vertebrae, the thoracic vertebrae, and the lumbar vertebrae - all segments that constitute bones in various regions of the spine; the cervical vertebrae are the bones that compose the uppermost region of the spine, the thoracic vertebrae are bones of the middle of the spine, and the lumbar vertebrae are the bones that the lowermost portion (Lumen Learning). I like to remember the lumbar region like lumber wood - just like how lumber can be used for baseboards, the bottommost part of a wall, lumbar is the lowest part of the spine!
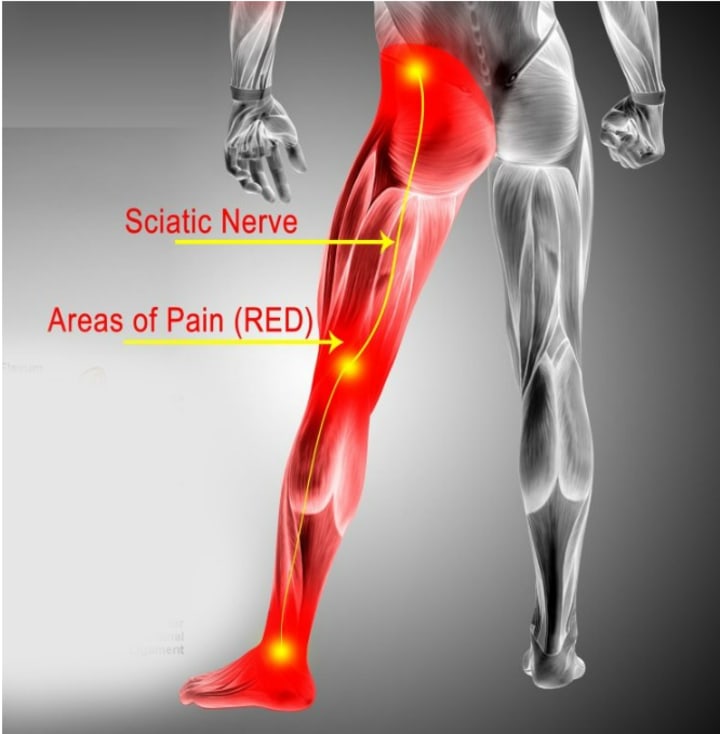
The latter half of the term, radiculopathy, refers to the origin point of nerve damage due to compression (Penn Medicine); thus, lumbar radiculopathy can be acknowledged as injury of a nerve from pressure and pinching stemming from the lumbar region of the spine; the pinched nerve here is the sciatic nerve, which runs from the lower back down to the end of the back leg, hence deriving the vernacular: sciatica.
What causes the pain?
As mentioned earlier, the sciatic nerve, the nerve running from the lumbar region of the spine down to the bottom of the leg, is damaged due to pressure and pinching, leading to nerve swelling or inflammation. Think of telephone - like, the game! Or, at least the version where you have a wire with two cans; two people each use a can and pass on a word - or messages - ‘through’ the wire to reach the other person.

Nerves work exactly like that! nerves are essentially wires in your body that send and receive messages to and from other parts of your body. When the nerve is disrupted, an improper message is sent or received; wouldn’t you be confused if you were playing the game and nothing made sense? Hearing gibberish from the messenger would be a problem, and this problem is equivalent to the major sciatic symptom: a confused nerve causes the body to interpret the message inefficiently, and it is translated into that sharp, shocking pain felt. Patients often have lower back pain, and since the nerve is acting slow, when patients try to stand up, shooting pain accompanies them - they may even have trouble walking and stepping forward if the nerve cannot relay the walking motion in time!
How does a nerve get pinched?
There are risk factors that amplify the probabilities of lumbar radiculopathy, including, but not limited to, prolonged sitting, physical stress, and age, but honestly, this breaks down to one factor: being alive (AAPM&R). Sorry, I don’t mean to be so morbid!
The longer an individual sits, the pressure from gravity and body weight can accrue and eventually crush the nerve over time, leading to sciatica symptoms. In terms of physical stress, events such as repeated lower back injuries, physical overexertion, and heavy lifting all increase susceptibility to having herniated disks(s) or slipped disk(s) - spongy cushion(s) - placed within your spine for structural support become misaligned through physical wear and tear (Cleveland Clinic, 2023). When the cushion is no longer appropriately placed and protruding, there may be collisions with the sciatic nerve, building a pinching sensation and gradually deteriorating the nerve (the telephone is broken!), leading to sciatica. As we age, our bodies and bones become more brittle - our discs and spine deteriorate in this process, leading to increased chances of developing herniated discs and sciatica. Combining all these factors, those most prone to having sciatica are middle-aged individuals, around 40-65 years of age, who have sedentary lifestyles and/or have physically strenuous work (Euro et al., 2019).
Diagnosis
Fortunately, medical advances and physician practice have enabled sciatica’s diagnosis. One test is called the Straight Leg Test (SLR). The SLR is not exclusive to sciatica and can be generalized for lower back pain diagnosis (Camino et al., 2019). At the doctor’s office, the SLR will require the patient to lie flat on their back and raise their leg - without any bend - until the patient complains of pain, indicating potential sciatica (Camino et al., 2019). This will feel different than just a normal stretch!

As for technological imaging, I would say that there are two main instruments: Computed Tomography and Magnetic Resonance Imaging, known as a CT (scan) and MRI, respectively. CT scans are similar to the panorama setting on your phone - they are multiple-angled pictures to get a 360-degree and three-dimensional high-detailed image of bone structure; you can think of CT scans as advanced X-rays since X-rays are just one picture from one angle and resultingly have lower bone density (Envision Radiology, 2019). On the other hand, MRIs use radio energy waves to produce images focused on soft tissues - the components that make up the body’s organs (Envision Radiology, 2019). A CT scan might help identify spinal degeneration or joint changes, such as spinal narrowing, while an MRI can give better detail on herniated discs from the collapse of the spinal discs - the spongy cushions - as they are a type of soft tissue (Carter, 2017).
General Treatment
Sciatica does dissipate over time, but measures may be taken to expedite the recovery process. While I am not recommending any products or medications myself, research shows that it is best to apply an ice pack in the first one to three days of the beginning of the irritation; honestly, it makes sense - ice helps to decrease swelling by decreasing blood flow in the affected area, which would be beneficial for an inflamed area (John Hopkins Medicine, 2022). For mobility, back braces may be worn at an individual’s choice; since the lower back is weakened and is not as supportive compared to being fully healthy, the back brace can assist pillar the body and reduce the effects of the pressure, partially potentially alleviating the discomfort while walking (WPH Physio, 2024). Choosing the right brace is also essential to the treatment (WPH Physio, 2024). Lastly, Over-The-Counter (OTC) painkillers - medicine that does not require a doctor’s prescription - may also aid in subsiding the pain, such as acetaminophen, commonly branded as Tylenol, or ibuprofen, commonly branded as Advil (WebMD, 2024).

But regardless of how one gets the condition, is diagnosed, or treated, the next time someone mentions it, inform them that it is lumbar radiculopathy - or will you still call it sciatica?






Comments
There are no comments for this story
Be the first to respond and start the conversation.