Finding Comfort: How to Manage Difficult Symptoms and Regulate Your System During Recovery Care
Managing Symptoms and Regulating Your System During Recovery
Recovery after colon cancer treatment can feel unpredictable. Often, food seems fine, but sometimes, it may cause side effects like nausea, urgency, or fatigue. That swing can make you doubt every choice you make. The good news is that small, consistent actions often create the biggest relief, especially when you focus on hydration, steady routines, and colon cancer nutrition treatment that supports healing instead of stressing your digestive system.
As you rebuild strength, your care team may also recommend follow-ups or adjustments based on symptoms. In some cases, they may discuss gastroenterology tests and procedures to clarify what is driving ongoing bowel changes, pain, bleeding, or difficulty eating. Knowing why those steps matter can help you feel less anxious and more prepared to advocate for yourself.
Additionally, read this post to learn more about managing difficult symptoms related to colon cancer and obtaining long-term recovery.

Common Side Effects After Colorectal Cancer Surgery
The recovery process after colorectal cancer surgery can vary depending on the type of procedure performed. If only polyps were removed, the recovery might be relatively quick, with minimal side effects. However, if part of the colon was removed to address cancerous tissue, there are typically more side effects to manage.
- Slow Bowel Movement: One of the most common side effects is a slow-moving bowel. This can happen due to anesthesia, pain medications, and the surgical intervention itself on the bowels. The digestive system may take some time to fully "wake up," a condition known as an ileus.
- Symptoms of Ileus: If you experience bloating, excessive gas, nausea, vomiting, or constipation lasting a couple of days, it could indicate the presence of an ileus. These symptoms are often temporary, but it's important to inform your surgeon if they persist longer than expected.
In most cases, your condition may resolve on its own within a few days, but if symptoms don’t improve, it’s essential to reach out to your healthcare provider for further evaluation.
What can you realistically control during recovery?
You cannot force your body to heal on a schedule, but you can make recovery easier to navigate. Focus on:
- Keeping hydration steady
- Building meals around protein and gentle carbs
- Using simple routines that reduce flare-ups
- Watching for red flags so you get help early
With that foundation, the next sections walk you through a practical plan, one symptom category at a time.
How can colon cancer nutrition treatment support healing when symptoms make eating hard?
Food is not just fuel right now. It is part of symptom control. After surgery or intensive treatment, your body needs extra energy and nutrients to repair tissue and recover.
That said, eating can feel like the hardest task of the day. Instead of pushing for perfect meals, aim for reliable, repeatable choices that your body tolerates.
What should you prioritize first: hydration, protein, or calories?
Start in this order because it prevents setbacks:
- Hydration: Dehydration can worsen fatigue, constipation, dizziness, and medication side effects.
- Protein: Supports healing and helps maintain muscle.
- Calories: Keep weight and energy from sliding too far.
If meals feel impossible, switch to mini targets: three small intakes per day that include protein, even if they are smoothies, soups, or yogurt bowls.
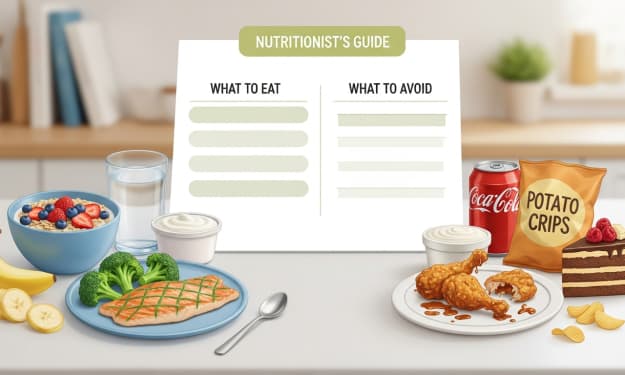
What should you eat when nausea, low appetite, or taste changes hit?
When appetite drops, make eating easier and more efficient:
- Eat small portions every 2 to 3 hours
- Choose softer textures when your gut feels sensitive
- Pick one protein anchor per mini-meal, such as eggs, Greek yogurt, lentils, tofu, fish, or chicken
- Adjust fiber based on symptoms: reduce rough, raw fiber during diarrhea or urgency, then reintroduce slowly once stools stabilize
If you want a simple food list to keep on hand, check this guide on the best nutrition choices and choose healthy foods that reduce your risk of colon cancer.
How can you approach managing symptoms during recovery in a simple daily plan?
Managing symptoms during recovery works best when you stop reinventing the day every morning. Routines reduce decision fatigue, and they often reduce symptom spikes too.
Start by choosing two daily anchors: one in the morning and one in the evening. Keep them simple enough that you can do them on low-energy days.
What should a recovery-friendly morning routine include?

A basic morning routine often helps digestion and energy settle:
- Drink water soon after waking
- Eat a small, protein-forward breakfast if possible
- Take a short walk or do gentle stretching to wake up your gut
Once you do this consistently, you can judge other changes more clearly because your baseline stays stable.
What does recovery care symptom management look like for bowel changes, gas, and urgency?
Recovery care symptom management becomes easier when you name the exact bowel pattern you have, because diarrhea and constipation need different strategies.
How can you respond to diarrhea in a safer, calmer way?
Diarrhea can dehydrate you quickly, so treat it as a priority symptom. NCI notes diarrhea is a common side effect of several cancer treatments, and it deserves proactive management.
Practical steps that often help:
- Sip fluids throughout the day instead of drinking large amounts at once
- Choose gentle foods short-term (soft carbs plus protein)
- Avoid greasy foods and very high-sugar items until stools stabilize
If diarrhea continues, worsens, or includes blood, call your clinician. Early guidance prevents complications.
How can you relieve constipation without making it worse?
Constipation can show up from pain meds, dehydration, reduced activity, or diet changes. MedlinePlus emphasizes drinking plenty of water and using laxatives only as your provider recommends.
Start with:
- Steady fluids
- Gentle movement
- Gradual fiber increases paired with water
If you have not had a bowel movement for several days or you develop significant pain, bloating, nausea, vomiting, or blood, contact a medical professional.
How to manage discomfort during recovery when pain and fatigue overlap?
How to manage discomfort during recovery often comes down to reducing the pain-fatigue loop. Pain disrupts sleep. Poor sleep makes pain feel louder. Breaking that cycle can make everything else easier.
How can gentle movement reduce fatigue without draining you?
You do not need intense workouts. Short, consistent movement often helps:
- bowel motility
- stiffness
- sleep quality
Start with five minutes of walking. Add a minute every few days if your body tolerates it.
What makes pain feel more predictable day to day?
Ask your care team about building a plan that matches your routine:
- Timing pain relief to support meals and sleep
- Using gentle heat or relaxation breathing when tension spikes
- Pacing activity so you move daily without triggering flares
- Even small adjustments can turn pain from constant to manageable.
What should you do at night to reduce tomorrow’s symptom stress?
Your evening routine should make tomorrow easier:
- Eat earlier when possible so your body can digest before sleep
- Prep one easy option for the next day, such as soup, oatmeal, or smoothie ingredients
- Do a one-minute check-in: what improved today, what worsened, what might have triggered it
That last step creates awareness without turning your life into a tracking project.
How do physical and emotional symptoms during healing affect your system, and what helps?
Physical and emotional symptoms during healing can amplify each other. When your gut feels unpredictable, anxiety rises. When anxiety rises, sleep and appetite often worsen. The goal is not to eliminate stress. It is to keep stress from driving your symptoms.
What can you do when anxiety spikes your symptoms?
Try a body-first reset that you can do anywhere:
- Breathe in for 4 seconds and out for 6 seconds for 3 minutes
- Sip water or a warm drink
- Take one next step: a small snack, a short walk, or a shower
This interrupts the spiral and gives your nervous system a steadier signal.
What sleep habits help regulate digestion and recovery?
Pick one sleep anchor and keep it consistent:
- Same bedtime window most nights
- Dim screens 60 minutes before bed
- A simple wind-down ritual, like light stretching
Better sleep often improves appetite cues and pain tolerance the next day.
What red flags mean you should call your doctor now?
Use clear thresholds instead of waiting it out:
- Fever: ACS defines fever for people with cancer as 100.4°F (38°C) or higher for at least one hour
- Severe abdominal pain, swelling, or inability to pass stool or gas
- Ongoing vomiting or inability to keep fluids down
- Blood in stool
- Rapid worsening of symptoms compared with your usual pattern
If something feels sharply different from your baseline, call even if you cannot explain why.
When do gastroenterology tests and procedures matter during recovery care?
Not every uncomfortable day needs testing. Still, ongoing or changing symptoms deserve evaluation because they can affect hydration, nutrition, and safety.
Common reasons a clinician considers follow-up include persistent diarrhea, new bleeding, escalating abdominal pain, or signs that you might not be passing stool or gas normally.
What should you bring to a GI visit so you get clearer answers?
A short, simple log helps your clinician connect the dots faster:
- Stool pattern (loose, formed, constipation, urgency)
- Your main symptom level is from 0 to 10
- What foods and medicines seemed to help or worsen things
- Any red-flag signs like fever, blood, vomiting, or severe pain
This keeps the appointment focused on decisions, not guesses.
Summing Up
Recovery feels easier when you stop trying to fix everything at once and start building steady supports. Prioritize hydration, protect protein intake, and use simple routines that reduce symptom spikes. Then bring clear notes to your appointments, so your team can guide you with precision.
Most importantly, treat colon cancer nutrition treatment as a practical recovery tool you use daily, not a perfect diet you must follow. Pick one change from this guide today, run it for three days, and keep what measurably improves comfort.
FAQs
What should I do if I cannot eat much, but I need strength to heal?
Shift from full meals to mini-meals every 2 to 3 hours, and include protein each time. Even small amounts add up. Focus on hydration first, then protein. If nausea or taste changes persist, ask your care team about medication timing, nutrition support, or a referral to a dietitian.
How do I know when bowel changes are normal versus a sign of a problem?
Some fluctuation is common during healing, but ongoing diarrhea, new bleeding, severe pain, or inability to pass stool or gas needs medical attention. If bowel changes block hydration or eating for more than a day or two, contact your clinician so you do not slip into dehydration or weakness.
Can stress really make recovery symptoms feel worse?
Yes. Stress can tighten your body, disrupt sleep, and reduce appetite, which can worsen pain and digestion. A short daily routine that includes hydration, a small walk, and a breathing reset often improves symptom stability, even when you cannot control everything else.
About the Creator
Erika Phillips
Erika Phillips, a dedicated Health content writer, crafts heartfelt, insightful articles. Passionate about the power of knowledge, she simplifies complex health topics, empowering readers to take charge of their well-being.




Comments
There are no comments for this story
Be the first to respond and start the conversation.