Dry Macular Degeneration Treatment: Exploring FDA Innovations
FDA Innovations in Dry Macular Degeneration Treatment

Living with dry macular degeneration can feel like watching the world slowly dim. Central vision, crucial for reading, driving, and recognizing faces, gradually blurs. For many years, treatment options were limited, focusing on slowing the disease's progression rather than halting or reversing its effects. However, the landscape is changing. Recent breakthroughs have led to new, FDA-approved therapies, offering renewed hope to millions. This article will explore these innovative treatments, explaining how they work and what they mean for people managing this condition.
Understanding Dry Macular Degeneration
Age-related macular degeneration (AMD) is a leading cause of vision loss for people over 50. It comes in two forms: wet and dry. The dry form is far more common, accounting for about 80-90% of all cases. It occurs when parts of the macula, the area of the retina responsible for sharp, central vision, get thinner with age. This process leads to the formation of small, yellow deposits called drusen under the retina. As the condition progresses, these deposits accumulate, and the light-sensitive cells in the macula gradually break down, resulting in a progressive loss of central vision.
The Stages of Dry AMD
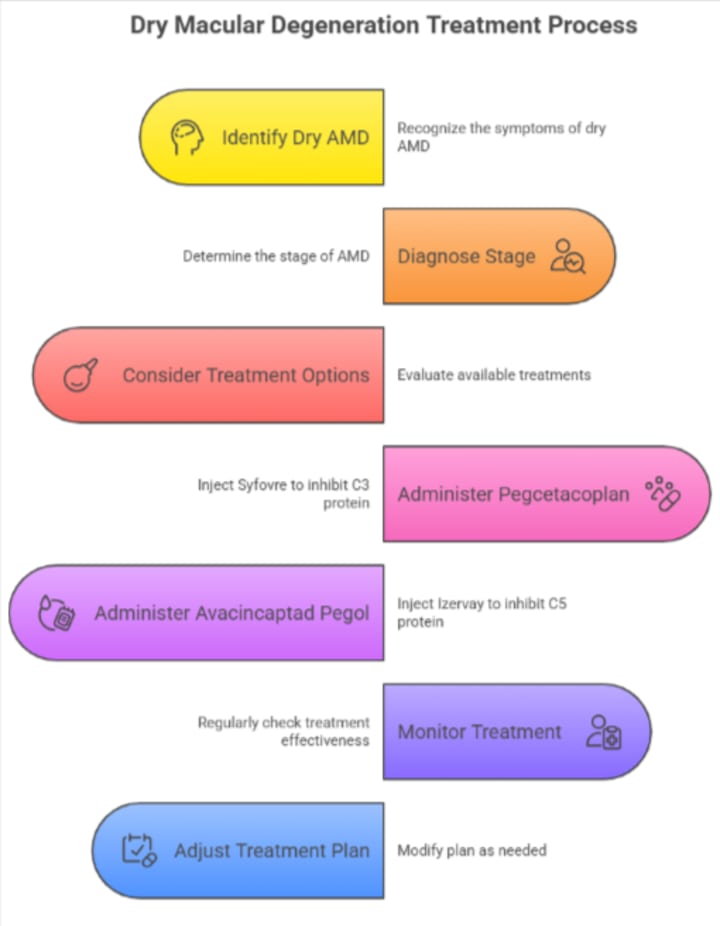
Dry AMD typically progresses through three stages:
- Early-Stage: Often, there are no symptoms. An eye doctor can detect medium-sized drusen during a comprehensive eye exam.
- Intermediate-Stage: Some people may notice mild blurriness in their central vision or find they need more light for reading. At this stage, drusen are larger.
- Late-Stage (Geographic Atrophy): In this advanced stage, there is a significant breakdown of light-sensitive cells and supporting tissue in the macula. This results in a noticeable blind spot in the central field of vision.
Until recently, management for dry AMD focused on nutritional supplements and lifestyle adjustments to slow its progression.
A New Era: FDA-Approved Treatments
For the first time, targeted treatments are available that address the underlying mechanisms of late-stage dry AMD, also known as geographic atrophy (GA). In 2023, the U.S. Food and Drug Administration (FDA) approved two groundbreaking drugs designed to slow the progression of GA. These therapies represent a significant leap forward in the dry macular degeneration treatment landscape.
Pegcetacoplan (Syfovre)
Approved in February 2023, pegcetacoplan was the first-ever treatment for geographic atrophy. It works by targeting a part of the immune system called the complement cascade. In dry AMD, an overactive complement system is thought to contribute to the damage and death of retinal cells.
- How it Works: Pegcetacoplan is a targeted C3 therapy. It binds to and inhibits the C3 protein, a central component of the complement cascade. By blocking this pathway, the drug helps reduce the inflammation and cell damage that drives the growth of GA lesions.
- Administration: The treatment is administered as an injection directly into the vitreous (the jelly-like substance in the middle of the eye) by a retina specialist. Injections are typically given every 25 to 60 days.
- Effectiveness: Clinical trials showed that pegcetacoplan significantly slowed the progression of GA lesions compared to a placebo. The effect increased over time, with greater reductions in lesion growth observed after two years of treatment.
Pro Tip: Regular follow-up appointments with your ophthalmologist are crucial when undergoing treatment for geographic atrophy. These visits allow your doctor to monitor the treatment's effectiveness, manage any potential side effects, and adjust the plan as needed to preserve your vision.
Avacincaptad Pegol (Izervay)
Following closely, avacincaptad pegol received FDA approval in August 2023. It also targets the complement cascade but focuses on a different protein within that system.
- How it Works: This drug is a C5 inhibitor. It blocks the C5 protein, which is further down the complement pathway. By inhibiting C5, avacincaptad pegol prevents the formation of a complex that causes inflammation and leads to the death of retinal cells.
- Administration: Similar to pegcetacoplan, this treatment is given as an intravitreal injection, typically administered on a monthly basis.
- Effectiveness: In clinical studies, avacincaptad pegol demonstrated a statistically significant reduction in the rate of GA lesion growth at 12 months compared to a placebo.
Comparing the New Treatments
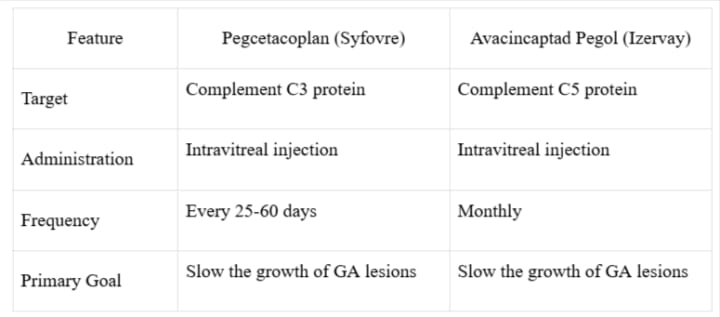
Both treatments are designed to slow the disease, not to reverse existing damage or restore lost vision. The goal is to preserve the vision you still have for as long as possible.
Quick Fact: According to the National Eye Institute, geographic atrophy affects over one million people in the United States. The availability of these new treatments marks a pivotal moment in the fight against this form of advanced dry AMD.
The Role of AREDS2 Supplements
While new injectable therapies target late-stage dry AMD, nutritional supplements remain the primary recommendation for patients with the intermediate stage of the disease. The Age-Related Eye Disease Studies (AREDS and AREDS2) found that a specific formula of vitamins and minerals can reduce the risk of intermediate AMD progressing to the advanced stage by about 25%.
The AREDS2 formula contains:
- Vitamin C (500 mg)
- Vitamin E (400 IU)
- Lutein (10 mg)
- Zeaxanthin (2 mg)
- Zinc (80 mg)
- Copper (2 mg)
It is essential to consult with an eye doctor before starting any supplement regimen to ensure it is appropriate for your specific stage of AMD.
Wrap-Up
The field of dry macular degeneration therapy has entered an exciting new phase. With the recent FDA approval of pegcetacoplan (Syfovre) and avacincaptad pegol (Izervay), patients with geographic atrophy now have options that can actively slow the progression of their condition. These therapies, which target the complement cascade, represent a monumental step forward from the previous approach of observation and nutritional support alone. While these treatments do not restore lost vision, they offer the invaluable gift of time—preserving existing sight and slowing the advance of the disease. For those with intermediate AMD, AREDS2 supplements continue to be a vital tool in reducing the risk of progression.
Key Takeaways
- Dry macular degeneration is a progressive eye disease that damages central vision.
- Until 2023, treatment was limited to nutritional supplements aimed at slowing progression in intermediate-stage AMD.
- Two new FDA-approved drugs, Syfovre and Izervay, are now available for late-stage dry AMD (geographic atrophy).
- Both drugs work by inhibiting parts of the complement system to slow the growth of retinal lesions.
- These treatments are administered via eye injection and aim to preserve existing vision, not restore what has been lost.
The FDA emphasizes the importance of targeting the complement system to effectively manage late-stage AMD. For further reading, visit the FDA's official page on AMD treatments.
FAQs
1. Who is a candidate for the new geographic atrophy treatments?
These new injectable treatments, Syfovre and Izervay, are specifically for patients diagnosed with geographic atrophy (GA), which is the late stage of dry macular degeneration. An eye care specialist can determine if you are a suitable candidate after a thorough examination.
2. Do these new treatments cure dry macular degeneration?
No, these treatments do not cure dry AMD. Their purpose is to slow the rate at which the disease progresses in its advanced stage. They help preserve the vision that a patient currently has, but do not reverse existing damage or restore lost vision.
3. Are there side effects to the new injectable treatments?
Yes, as with any medical procedure, there are potential side effects. The most common ones include eye discomfort, floaters, and bleeding at the injection site. More serious but rare risks include eye infection (endophthalmitis) and inflammation. Your retina specialist will discuss all potential risks with you.
About the Creator
Franklin Norton
Franklin Norton is a dedicated health writer specializing in eye care. With a passion for vision health, he educates readers on eye conditions, treatments, and preventive care for optimal eye wellness.






Comments
There are no comments for this story
Be the first to respond and start the conversation.