A Formal Analysis Of A Case-Control Study Focused On The Sleeping Behaviours Of Children Diagnosed With Smith-Magenis Syndrome (SMS)
A close look at a study analyzing how a rare genetic condition limits melatonin production and causes sleep abnormalities in clinically diagnosed children with prospect on how to remedy the issue
When I was five years old my aunt had her first son. When he was born, he had a plethora of minor health issues and as he grew up, his parents and family noticed that he had behavioral differences and struggled with important aspects of life such as sleeping, cognition and health problems. My aunt brought him to the hospital frequently until they finally diagnosed him with Smith-Magenis Syndrome (SMS). Since that day they have been on the hunt for various ways he can be treated to alleviate the difficulties of the condition. When I was fourteen my sister and I held a bake sale concerning PRISMS, the foundation dedicated to furthering research on Smith-Magenis syndrome. It is an American-based foundation as there are no Smith-Magenis foundations in Canada. It is a condition that is deemed very rare, and therefore it is hard to find proper treatment and support, especially in Canada. One thing I always noticed is that my cousin does not sleep very well. He often wakes up throughout the night and won’t sleep for more than a few hours, frequently waking up every day at 5 am. I have always been curious about furthering my knowledge on the condition and ways to help my cousin, therefore I will be looking at a case-control study that looks at the sleeping habits of children diagnosed with Smith-Magenis Syndrome.
What Is Smith-Magenis Syndrome?
Smith-Magenis Syndrome is a complex genetic condition that causes intellectual disability, behavioral issues and other health issues. It is caused by a chromosomal deletion or functionality problem on chromosome 17p11.2 (NORD - National Organization for Rare Disorders, 2017). Chromosome 17 varies in characteristics from the others as it has the second highest density out of all the chromosomes. This is because chromosome 17 is rich in protein-coding genes. Because of chromosome 17’s intricate rearrangement and duplication structure it predisposes it to non-allelic homologous recombination (NAHR) which leads to the DNA rearrangements that cause several well-studied microdeletion disorders like Smith-Magenis Syndrome (Zody et al., 2006). Since this chromosome is either deleted or non-functional, it does not code for the important proteins that promote human cell regulation and development. The RAI1 gene is the exact protein associated with Smith-Magenis Syndrome. Since there is an insufficient production of RAI1, also known as retinol acid-induced 1, it leads to defects that are the cause of the behavioral, temperamental, emotional and clinical issues seen in individuals with the condition (Falco et al., 2017). Since this condition affects chromosome 17, it is haploinsufficient in individuals with Smith-Magenis Syndrome. Chromosome 17 is an essential part of the transcription of the circadian locomotor output cycles kaput, commonly known as the CLOCK gene (Trickett et al., 2020). The CLOCK gene is responsible for the regulation of the circadian rhythm, therefore causing the characterizing of sleep abnormalities in individuals with Smith-Magenis Syndrome.
What Data Were They Looking For?
This study aimed to use actigraphy data to compare the temporal analysis of the brain activity of children with SMS and developing children without the condition (Trickett et al., 2020). This study was formulated on the foundational knowledge of the relationship between Smith-Magenis syndrome and circadian rhythm. A part of the condition is that it creates sleep abnormalities and irregular circadian rhythm. This study uses Smith-Magenis diagnosed children and age-matched control children to compare their circadian rhythm patterns and the impact of day-time sleepiness and inefficient sleep patterns on a child's brain. An actigraphy is a type of device that can be easily worn by children for a certain period to measure factors such as the time one falls asleep, the time one wakes up, the duration it takes one to fall asleep, the duration of one's total sleep and the amount of waking hours one experiences after falling asleep beforehand (Pacheco & Singh, 2021). Temporal analysis is conducted by comparing the data collected by the actigraphy to analyze the different effects of sleepiness and the duration of sleep concerning behavior over different periods in a day.
What Factors Did They Focus On And Find?
In this study, they restricted it to children that ranged from four to fifteen years old. They recruited 26 children to participate in this study, yet six children could not handle using the actigraphy watch for more than a few nights, therefore this is a case-control study that focuses on twenty children, ages four to fifteen clinically diagnosed with Smith-Magenis Syndrome. They then age-matched 45 controls to be compared to the exposed/diagnosed group of children. Their first order of business was to administer a questionnaire to all of the parents of the children in this study to be filled out. This questionnaire included questions about family income and medication use, focusing on melatonin supplements. They found no significant differences between families with different incomes as well as children who took melatonin supplements to be significant factors in this study. When analyzing the actigraphy data of the exposed/diagnosed group and comparing it to the control group, the children with Smith-Magenis Syndrome had far earlier morning wake times, shorter sleep duration and a large number of nightly waking periods than compared to the control children. Out of the children diagnosed with Smith-Magenis Syndrome, 95% of the children partake in diurnal napping (daytime napping) while only 10% of the control children took diurnal naps. The mean for the exact time at which the children with Smith-Magenis Syndrome took their naps had a mean of 90% across the duration of study time, meaning the time varied among the days. They also found a negative relationship between total sleep time and diurnal naps which may be why they also saw that children with Smith-Magenis Syndrome tended to go to bed earlier than the control group. When looking at daytime sleepiness in children, 76.5% of the children with Smith-Magenis Syndrome suffered from this compared to zero percent of the control group. The sleeping tendencies of the children in the control group varied depending on their age, while the children with Smith-Magenis Syndrome had no significant correlation in regards to a relationship between age and the duration of sleep, yet the time at which individuals went to bed became later with the increasing of age amongst both groups.
What Relationships Did This Case-Control Study Lead Them To Find?
In this study, multiple factors associated with sleep were found to be very impactful. Descriptive statistics were used to measure the significance of these findings. A p-value of >0.05 was deemed significant, with an alpha value set at <0.01 to decrease the chance of type I error among the variables. Attached below is a mixed linear model taken directly from the study, modeling the relationships they found and how they work together in the children with Smith-Magenis Syndrome when compared to the control group.
Figure 3. From Trickett et al., 2020 Study Showing The Relationships Found Between Sleeping And Behaviour In Children With Diagnosed Smith-Magenis Syndrome
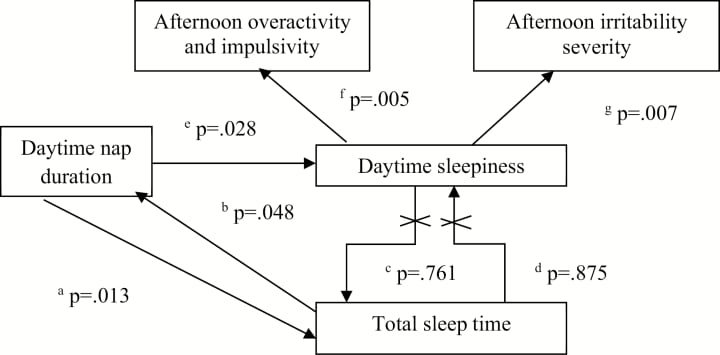
This model demonstrates the interpersonal relationships between the findings from this study and their significance. This model shows how longer nap time duration caused a shorter duration of sleeping from the start of bedtime and shorter sleep during the night added to the duration of nap time the next day. Some relationships were found to be irreversible and only worked forwards. With this, daytime sleepiness did not predict the total sleep time of the children that night and total sleep time did not work in predicting daytime sleepiness in the individuals as well. The duration of daily naps was found to have an impact on the sleepiness of the children and played into behavioral problems. Higher levels of sleepiness were found to be directly correlated to the irritability and impulsivity of the children.
What Does This Information Tell Us And How Can We Apply It?
Using the knowledge on Chromosome 17 and its effect on circadian rhythm, these researchers compared factors that have never been compared in Smith-Magenis Syndrome individuals. The main overall findings of this study were how interconnected all aspects of the condition are regarding sleep. The behavioral problems of individuals with Smith-Magenis Syndrome worsened with the decrease in sleep, leading to daytime sleepiness. The scientists of this study suggested that proper hygiene before bed and creating a routine may have a greater impact on the amount of nocturnal sleep an individual with Smith-Magenis may get in a night. Another method they suggested was to use morning beta-blockers to minimize melatonin production during waking hours. These are two optimal suggestions as when combined, they can help increase nocturnal sleep in individuals, which is what leads to daytime sleepiness as well as eliminate melatonin production to fix the circadian rhythm, eliminating daytime sleepiness. These two factors together would benefit individuals significantly, correcting sleeping patterns and in turn helping with behavioral issues.
Conclusion & Take Aways
Since I have personal experience with this condition, analyzing this case-control study was very insightful. My cousin suffers from these sleep problems, and the idea of blocking melatonin production during the day seems like a very integral concept. To add to their suggestions, I would also suggest a controlled home environment for individuals with Smith-Magenis Syndrome. A relaxed, calm environment and the use of these tools could really benefit these children suffering from this condition. After reading the information about the genetics and issues with Chromosome 17, RAI1 and the CLOCK gene, there is hope that modern technology could help remedy individuals. Possibly in the case of individuals with a damaged chromosome 17 and not entirely missing, modern gene editing tools (ex. CRISPR-Cas9) could be developed and used to promote the regulation of the proteins associated with it. There is still a lot of research that needs to go into alleviating these individuals, but with the use of modern medicine like gene editing tools and furthering the research of these rare conditions, there is hope for treatments to help these patients.
References
NORD - National Organization for Rare Disorders. (2017, June 23). Smith Magenis Syndrome. NORD (National Organization for Rare Disorders). https://rarediseases.org/rare-diseases/smith-magenis-syndrome/
Zody, M. C., Garber, M., Adams, D. J., Sharpe, T., Harrow, J., Lupski, J. R., Nicholson, C., Searle, S. M., Wilming, L., Young, S. K., Abouelleil, A., Allen, N. R., Bi, W., Bloom, T., Borowsky, M. L., Bugalter, B. E., Butler, J., Chang, J. L., Chen, C. K., Cook, A., … Nusbaum, C. (2006). DNA sequence of human chromosome 17 and analysis of rearrangement in the human lineage. Nature, 440(7087), 1045–1049. https://doi.org/10.1038/nature04689
Falco, M., Amabile, S., & Acquaviva, F. (2017, November 3). rai1 gene mutations: Mechanisms of Smith-Magenis syndrome. The application of clinical genetics. Retrieved November 14, 2022, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5680963/
Trickett, J., Oliver, C., Heald, M., Denyer, H., Surtees, A., Clarkson, E., Gringras, P., Richards, C., Sleep in children with Smith–Magenis syndrome: a case–control actigraphy study, Sleep, Volume 43, Issue 4, April 2020, zsz260, https://doi.org/10.1093/sleep/zsz260
Pacheco, D., & Singh, A. (2021, October 1). How Is Actigraphy Used to Evaluate Sleep? Sleep Foundation. https://www.sleepfoundation.org/sleep-studies/actigraphy
About the Creator
Marisa Chiaravalloti
Hello, I am an Honours Biomedical Science student with a Minor in English curious about all things science. I am also the primary writer and researcher for the TMU Rare Diseases Club's online educational section. I hope you enjoy! 🔬







Comments
There are no comments for this story
Be the first to respond and start the conversation.