Lewy Body Dementia: 7 Stages, Symptoms & Care Guide
Your essential guide to recognizing and responding to each stage of Lewy Body Dementia.
Lewy Body Dementia is the second most common form of progressive dementia after Alzheimer’s. It’s caused by the buildup of Lewy bodies—abnormal protein deposits in the brain—that affect thinking, movement, behavior, and sleep.
Unlike Alzheimer’s, LBD has unique symptoms like fluctuating cognition, vivid hallucinations, and motor problems similar to Parkinson’s disease. Though a small number of cases may be genetic, most are not inherited. Understanding the seven stages of Lewy Body Dementia helps caregivers plan ahead and manage symptoms better.
“LBD is challenging to diagnose due to its changing symptoms. Early recognition supports better treatment.” — Dr. Sarah Chen, Johns Hopkins Medical Center
The 7 Stages of Lewy Body Dementia
Stage 1: No Noticeable Symptoms
- Brain changes start, but there are no clear signs yet.
- Best time for future planning and healthy habits.
Stage 2: Very Mild Changes
- Minor memory lapses or personality shifts.
- Often mistaken for normal aging.
Stage 3: Mild Cognitive Issues
- Planning and memory challenges become more obvious.
- Early hallucinations and attention changes may begin.
Stage 4: Moderate Decline
- Help needed with daily tasks like cooking or handling money.
- Hallucinations become more frequent; motor symptoms may appear.
- Often when diagnosis is made.
Stage 5: Moderately Severe Decline
- Memory loss worsens; help needed for basic self-care.
- Sleep and mobility problems increase.
- Start discussing long-term care options.
Stage 6: Severe Decline
- Needs full assistance with daily activities.
- May not recognize loved ones; increased behavioral and health risks.
Stage 7: Very Severe Decline
- Limited speech and mobility.
- Requires round-the-clock care.
- Focus shifts to comfort and end-of-life support.
LBD vs. Other Dementias
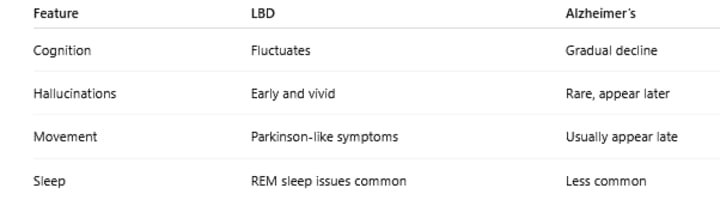
“LBD affects thinking, movement, mood, and sleep, so care must be holistic.”— Dr. Michael Rodriguez, Mayo Clinic
Treatment Options by Stage
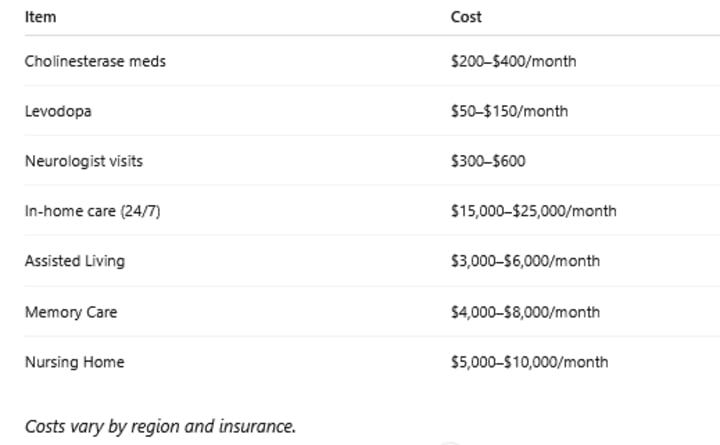
While there is no cure, several treatments can improve quality of life:
Medications:
- Cholinesterase inhibitors (donepezil, rivastigmine): Improve thinking in early stages.
- Avoid typical antipsychotics: They can worsen LBD symptoms.
- Levodopa: Helps with movement but may increase confusion.
- Melatonin: Eases sleep issues.
Therapies:
- Physical therapy: Maintains mobility.
- Occupational therapy: Supports independence.
- Speech therapy: Helps with communication and swallowing.
- Cognitive stimulation: Keeps the mind engaged.
Cost Overview (Approximate)
Managing Behavioral Symptoms by Stage
- Early Stages (1–3): Keep routines consistent, reduce stress, and provide reassurance.
- Middle Stages (4–5): Manage hallucinations calmly; introduce structured activities and consider adult day programs.
- Advanced Stages (6–7): Prioritize comfort, prevent infections, and prepare for end-of-life care.
Family & Caregiver Support
Caring for someone with LBD is emotionally and physically demanding. Support includes:
- Educational tools and caregiver guides
- LBD-specific support groups
- Legal and financial planning resources
- Respite care to avoid burnout
Plan early—ideally in stages 1–3—when the individual can participate in decision-making.
Recent Advances in LBD Research (2023–2025)
- Earlier diagnosis using biomarkers
- VR cognitive training with measurable benefits
- Personalized treatments via precision medicine
- Improved REM sleep treatments
- Antioxidants showing promise in slowing disease progression
“Advances in early diagnosis and targeted treatments offer real hope for LBD patients.” — Dr. Jennifer Walsh, National Institute on Aging
When to Seek Medical Help
- Get professional help if you notice:
- Sudden behavior or mood shifts
- New or worsening motor symptoms
Medication side effects
- Safety risks (e.g., driving, cooking)
- Signs of depression or aggression
- Caregiver Checklists by Stage
Stages 1–2:
- Begin legal and care planning
- Join support groups
- Assess home safety
Stages 3–4:
- Set routines
- Monitor medication
- Start therapies
- Consider adult day programs
Stages 5–7:
- Arrange long-term or palliative care
- Provide 24/7 support
- Monitor for infections and swallowing problems
Conclusion
Lewy Body Dementia unfolds in seven stages, but each person’s experience is unique. Some progress quickly; others remain stable for years. Understanding the stages helps families plan ahead, adapt care, and maintain quality of life.
Stay focused on current needs, use available resources, and don’t hesitate to seek professional help. With the right support, meaningful connections and quality care are still possible—even in the later stages of this complex condition.
About the Creator
PURE HEALTH BLOGS
Pure Health Blogs offers expert tips on general health, beauty, fitness, nutrition, mental wellness, and recipes. We help you live healthier every day with science-backed insights and practical advice.






Comments
There are no comments for this story
Be the first to respond and start the conversation.