Are Weight Loss Injections the Future of Obesity Treatment or Just Another Billion-Dollar Trend?
How GLP-1 Drugs Are Reshaping Medicine, Body Image, and the Business of Health
A weekly injection.
A quieter appetite.
A body that finally begins to respond.
For someone who has battled weight for years, that is not vanity. That is relief.
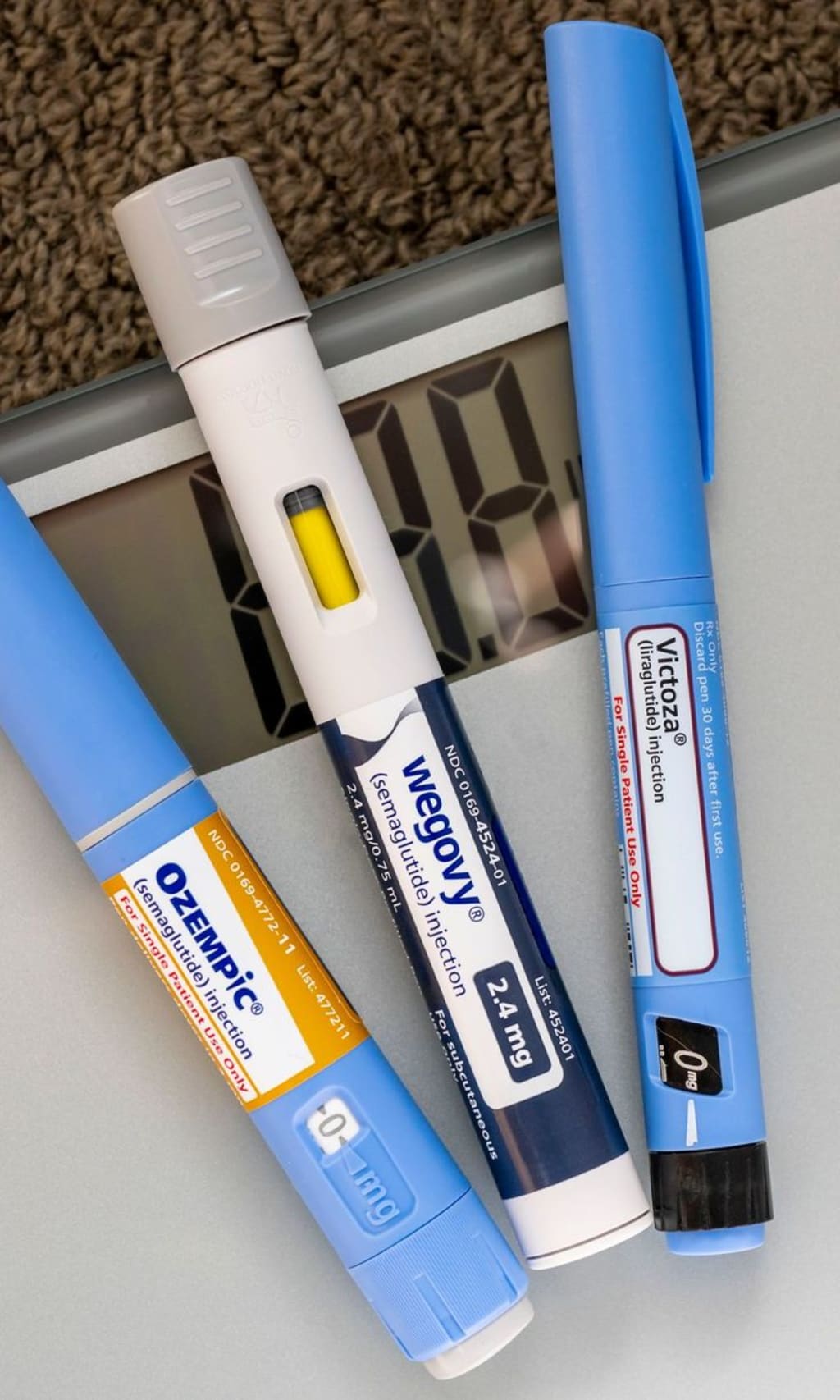
Across the United States, medications like Ozempic, Wegovy, and Mounjaro have moved from endocrinology offices into everyday conversation. What began as treatment for type 2 diabetes has evolved into one of the most transformative and controversial developments in modern medicine.
Scroll through social media and you will see dramatic transformations. Listen to health podcasts and you will hear debates about ethics, safety, and cost. Sit in a primary care clinic and you will hear something different: exhaustion.
Patients who have tried diets, workouts, calorie tracking, fasting, and every trending program available. Patients who feel blamed for a disease that science now recognizes as deeply biological.
So the real question is not simply whether these drugs work.
It is what they represent.
America’s Obesity Crisis: More Than a Statistic
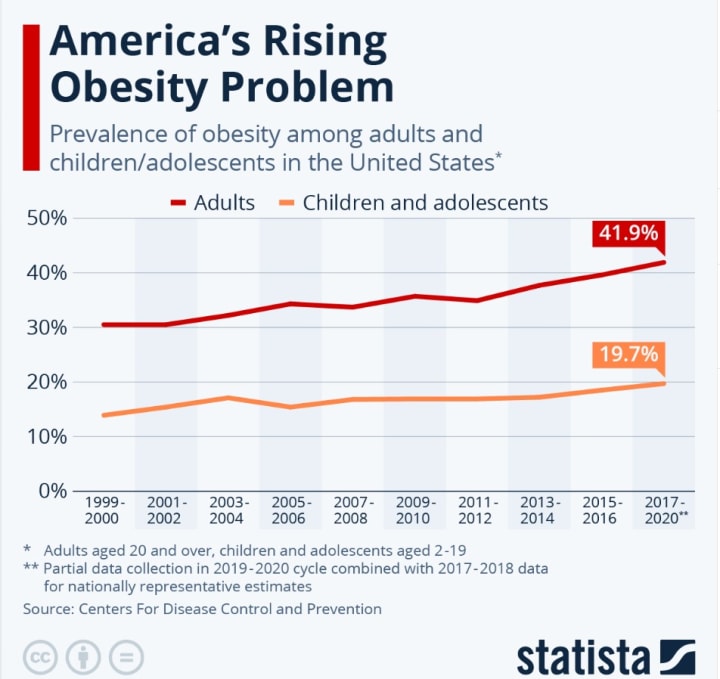
More than 40 percent of American adults are classified as obese. Severe obesity continues to rise, particularly among younger populations.
But numbers do not show the lived experience.
Obesity in the United States is closely tied to:
- Type 2 diabetes
- Cardiovascular disease
- Hypertension
- Stroke
- Certain cancers
- Reduced life expectancy
It is also tied to stigma, bias, and quiet shame.
For decades, the dominant narrative framed weight as a personal failure. Eat less. Move more. Try harder.
Yet long-term studies repeatedly show that sustained weight loss through lifestyle change alone is extraordinarily difficult for many individuals. This is not because people lack discipline. It is because obesity involves hormonal signaling, brain reward pathways, insulin resistance, genetics, and environmental triggers.
Highly processed foods are engineered for palatability. Work environments are sedentary. Many communities lack safe spaces for exercise or access to fresh food.
When we talk about obesity, we are not just talking about calories. We are talking about biology colliding with environment.
That is where GLP-1 medications enter the discussion.
The Science: A Shift in Understanding Hunger
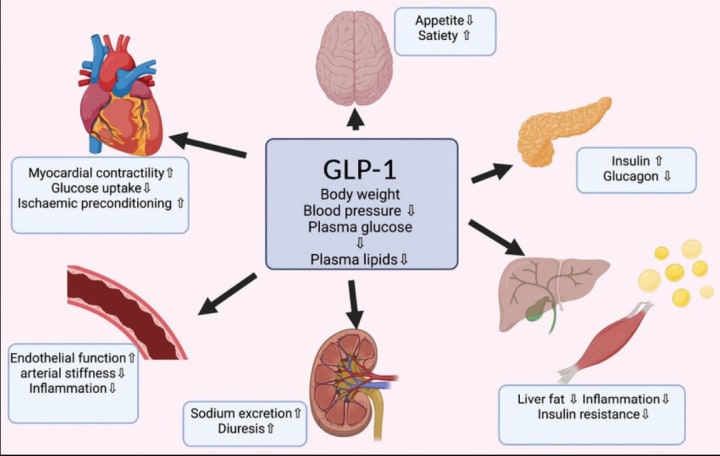
GLP-1 receptor agonists mimic a hormone called glucagon-like peptide-1, which plays a central role in appetite regulation and blood sugar control.
These medications:
- Slow gastric emptying
- Reduce hunger signals in the brain
- Increase satiety
- Improve insulin response
In clinical trials, patients have experienced average weight reductions of 10 to over 20 percent of total body weight, depending on dosage and duration.
From a medical perspective, this is groundbreaking.
A reduction of even 5 to 10 percent in body weight can significantly lower blood pressure, improve cholesterol profiles, and reduce the risk of developing type 2 diabetes. For some patients, it can mean avoiding insulin therapy or delaying cardiovascular complications.
This is not cosmetic weight loss. This is metabolic intervention.
For the first time, many patients report that the constant “food noise” in their minds quiets. Hunger feels manageable. Portion control no longer feels like a daily battle.
That psychological relief cannot be dismissed. For some, it feels like their biology is finally cooperating instead of resisting.
The Complicated Reality
But progress often arrives with complexity.
Common side effects include:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Fatigue
Some individuals experience significant gastrointestinal distress, especially during dose escalation. More serious but less common concerns include pancreatitis, gallbladder disease, and potential thyroid-related risks. Long-term safety data is still being collected.
There is also the issue of dependency. Studies show that when patients discontinue GLP-1 medications, much of the lost weight may return.
This reframes the conversation.
Are these drugs a short-term boost, or are they chronic disease management tools that require lifelong use?
If obesity is treated like hypertension or diabetes, long-term medication is not unusual. Yet the financial burden complicates this reality. Without insurance coverage, monthly costs can range from several hundred to over a thousand dollars.
Access is uneven. Shortages have occurred, sometimes affecting diabetic patients who depend on these medications for blood sugar regulation.
The question becomes not only medical, but ethical.
Who receives treatment?
Who waits?
Who profits?
The Business of Weight
The economic dimension cannot be ignored.
The market for GLP-1 medications is projected to reach tens of billions of dollars globally. Pharmaceutical companies are investing aggressively in research, expansion, and marketing.
When a drug intersects with both medical necessity and cultural desire, the commercial potential multiplies.
Weight loss has always been a lucrative industry. From diet programs to supplements, billions have been spent on promises. The difference now is that the results are scientifically measurable.
But commercialization carries risks.
If prescriptions are driven by aesthetic demand rather than medical necessity, we risk shifting from therapeutic innovation to consumer trend. If social pressure drives usage, we may amplify body image anxiety rather than resolve metabolic disease.
We must ask whether the framing of these medications emphasizes health or appearance.
There is a difference between reducing cardiovascular risk and shrinking to meet societal standards.
My Perspective: Tool, Not Salvation
I do not view weight loss injections as a miracle cure. Nor do I see them as a reckless fad.
They are powerful medical tools, and for many patients with obesity-related disease, they may represent one of the most significant advances in treatment in decades.
But tools require context.
An injection cannot replace:
- Nutritional education
- Behavioral counseling
- Psychological support
- Community health reform
- Policy changes addressing food systems
Obesity in America is shaped by economic inequality, food marketing practices, urban design, and healthcare access. These medications treat biology. They do not correct structural imbalance.
If we rely solely on injections, we risk treating symptoms while leaving systemic causes untouched.
Yet dismissing these medications would also be irresponsible. For individuals whose health is deteriorating under the weight of metabolic disease, these drugs may extend life, prevent complications, and restore mobility.
The key is balance.
Science should guide use. Ethics should guide access. Compassion should guide conversation.
Looking Forward
Weight loss injections may indeed be part of the future of obesity treatment. The evidence is compelling. The demand is real. The health implications are significant.
But the future of obesity care cannot be reduced to a syringe.
It must include prevention, education, structural reform, and individualized medical treatment working together.
The true measure of progress will not be how quickly numbers drop on a scale.
It will be whether we create a healthcare system that treats obesity as a complex chronic disease while protecting patients from exploitation, stigma, and inequality.
The injections are powerful.
The responsibility to use them wisely is even greater.
******
Thank you for taking the time to read and reflect on this discussion. I welcome thoughtful perspectives, professional insights, and respectful dialogue in the comments. Conversations like these help us move beyond headlines and toward deeper understanding.
At the moment, I am unable to respond directly to comments due to platform restrictions. However, I truly value your engagement and will do my best to address important questions and perspectives in my next post. I hope this issue will be resolved soon so I can interact more actively with you all.
If you are interested in exploring more about nutrition and public health shifts, you may also enjoy my article The Food Pyramid Has Been Flipped. Here’s What the New One Really Means — click here to read more.
About the Creator
Aarsh Malik
I WAS SILENCED
Comments are temporarily suspended due to platform limitations.
Poet, Storyteller, and Healer.
Sharing self-help insights, fiction, and verse on Vocal.
Anaesthetist.
...






Comments (4)
this was so refreshing. i am unable to take glp-1 medications because i have osteoporosis and apparently the meds can do a number on bone density. but i would likely be taking them if that weren't an issue. my family health history is riddled with diabetes and obesity related heart disease. they probably could have helped several members of my family if they had been around. "Science should guide use. Ethics should guide access. Compassion should guide conversation." spot on. thanks for this 💙
Thank you my friend. LOVE IT
I refuse to take shots. I eat only one meal a day. I eat whole foods, no processed foods. No junk food. No sugar. No rice. No bread. I exercise a lot. I have many black belts. I was a gymnast growing up.
HELL NO>