Why Can’t Many Patients with Chronic Prostatitis Hold Their Urine? Simple Science, Real Relief
Urinary urgency explained—what’s driving it, what helps, and where herbal support like the Diuretic and Anti-inflammatory Pill may fit.
A familiar story you might recognize
You’re stuck in traffic or halfway through a meeting when it hits: the sudden, can’t-wait urge to pee. You went not long ago, and yet your bladder feels like it’s sounding an alarm. If this sounds familiar, you’re not alone—and if you live with chronic prostatitis or chronic pelvic pain syndrome (CP/CPPS), urinary urgency and frequency can be some of the most frustrating symptoms.
Let’s unpack why this happens and what you can do today to reclaim control.
Why can’t many patients with chronic prostatitis hold their urine?
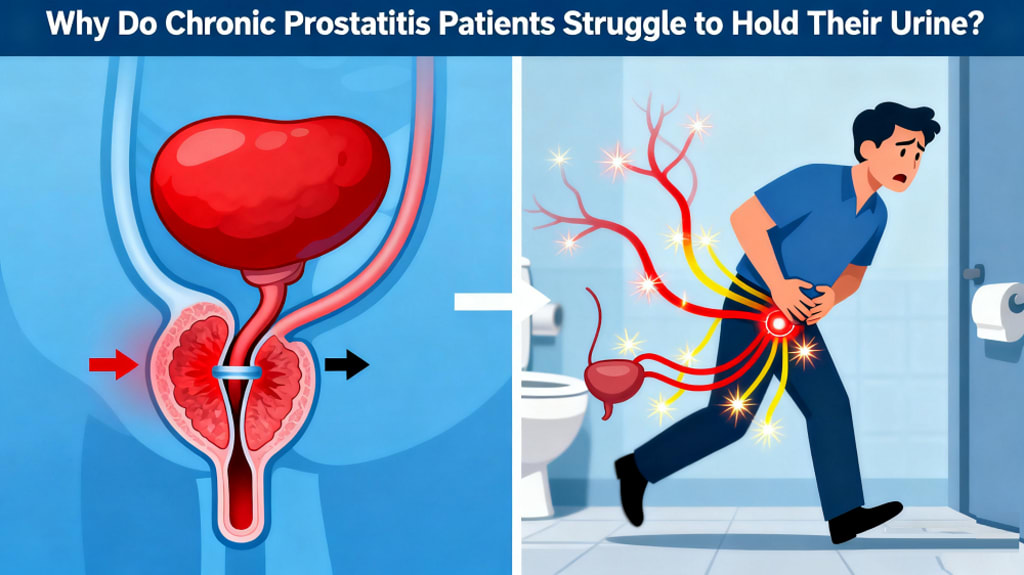
Chronic prostatitis (often part of CP/CPPS) isn’t just a “prostate problem.” It’s a complex condition where the prostate, bladder, pelvic floor muscles, and nervous system all share space—and sometimes share irritation. Think of your pelvic area like a crowded neighborhood: if one house has a loud party (inflammation, muscle tension, or nerve irritation), the whole block hears it.
Key reasons urgency shows up:
Local inflammation and sensitivity: Even when there’s no active infection, lingering inflammation can make bladder and prostate nerves overly sensitive. That means normal bladder filling triggers an outsized “must go now” signal.
Pelvic floor muscle tension: When the pelvic floor—the sling of muscles that help control urine—stays tight from pain or guarding, it becomes a faulty “brake.” A tight brake can paradoxically make urgency worse and keep the bladder from fully relaxing and emptying.
Bladder/prostate cross-talk: The bladder and prostate sit close together and share nerve pathways. Irritation in one can amplify signals in the other, creating a feedback loop of urgency and frequency.
Stress and the “fight-or-flight” effect: Stress ramps up the sympathetic nervous system, which can increase muscle tension and sensory sensitivity. Many people notice urgency flares during stressful weeks.
Prostate vs. bladder: what’s really going on?
There are different “flavors” of prostatitis:
Chronic bacterial prostatitis: Fewer cases. Caused by recurring infection. Urinary symptoms plus burning, sometimes fever. Needs antibiotics guided by a clinician.
CP/CPPS (nonbacterial): Most common. Pain in the pelvis, perineum, lower back, or genitals, plus urinary urgency/frequency. It’s multifactorial—muscles, nerves, and inflammation all play roles.
So when you’re wondering, “Why can’t many patients with chronic prostatitis hold their urine?”, the answer is rarely just one thing. It’s often a mix of sensitized nerves, irritated tissues, and tight muscles feeding into each other.
Everyday habits that make urgency worse (and what to try instead)
Small changes can make a big difference. Try these:
Cut bladder irritants for 2–3 weeks: Caffeine, alcohol, energy drinks, carbonated beverages, and very spicy or acidic foods can ramp up urgency. Reintroduce slowly to spot triggers.
Hydration “windows”: Don’t chug water all morning, then go dry; that swing can provoke urgency. Aim for steady sips, about 1.5–2 liters daily unless your doctor advises otherwise. Ease off an hour or two before bedtime.
Warmth helps: A warm sitz bath or heating pad across the lower abdomen or perineum can relax muscles and soothe irritated nerves.
Gentle movement: Walking, yoga, or stretching eases pelvic tension. Avoid long bike rides or heavy squats during flares if they worsen symptoms.
Manage constipation: A backed-up bowel presses on the bladder and pelvic nerves. Add fiber (fruits, veggies, oats), fluids, and movement.
How doctors figure it out
If urgency is new, severe, or worsening, a urologist or primary care clinician can rule out infection or other issues. Common checks include:
Urinalysis and urine culture (plus STI screening if relevant)
Digital rectal exam to assess prostate tenderness and size
Post-void residual (ultrasound or scan) to see if you’re emptying fully
Symptom questionnaires to track severity and guide treatment
What actually helps the urge—today and long-term
Quick wins for immediate relief:
Urge suppression technique: When the urge hits, stop, stand tall, do 5–10 quick pelvic floor “squeezes” (think lifting the area you’d contract to stop urine), then slow belly breaths. Often the urge settles enough to wait a few minutes.
Timed voiding: Start with scheduled bathroom breaks every 2–3 hours. Gradually extend the interval by 10–15 minutes every few days. This retrains the bladder’s “alarm system.”
Breathing down the belly: Inhale for 4, exhale for 6–8. Longer exhales calm the nervous system and reduce pelvic guarding.
Therapies and medicines your clinician may suggest:
Pelvic floor physical therapy: Gold-standard for CP/CPPS. Therapists help release muscle tension, improve coordination, and teach habits that reduce urgency and pain.
Alpha-blockers (e.g., tamsulosin): Relax bladder neck and prostate smooth muscle, easing flow and urgency for some patients.
Anti-inflammatories: Short courses may help during flares, used under guidance.
Neuromodulators (low-dose tricyclics or gabapentinoids): In select cases, these calm overly sensitive nerves.
Antibiotics: Only if there’s confirmed bacterial prostatitis. Taking them “just in case” can backfire.
Evidence-informed supplements: Some men report relief with quercetin or pollen extracts; results vary and should be discussed with your clinician.
Where a herbal option may fit: Diuretic and Anti-inflammatory Pill
Many readers ask about herbal support for urinary frequency and pelvic discomfort. One option used in Traditional Chinese Medicine is the Diuretic and Anti-inflammatory Pill. It’s formulated to support urinary flow, ease pelvic inflammation, and may help reduce urgency in some individuals. If you’re considering it:
Integrate thoughtfully: Herbal support can be a complement to lifestyle changes and physical therapy. It’s not a substitute for antibiotics when infection is present.
Talk to your clinician: Check for interactions with current medications, and ensure it’s appropriate for your health history.
Buy from reputable sources: Quality matters with herbal products.
Set realistic expectations: Benefits can be gradual and vary person to person.
Why can’t many patients with chronic prostatitis hold their urine? A nerve-and-muscle story
In short, urgency is often a “volume knob” problem, not just a “full tank” issue. Sensitized bladder nerves amplify signals, while tight pelvic muscles keep the system on guard. The good news: nerves and muscles are trainable. With consistent habits, targeted therapy, and appropriate medical care, many people experience real improvements.
When to seek urgent care
Call your clinician promptly if you have:
Fever, chills, or feeling very unwell
Burning urine with blood, or severe pain in the back/flank
Inability to urinate (or significant retention)
New numbness or weakness in the legs, or severe neurological symptoms
Your action plan for this week
Start a bladder diary: Track fluid intake, triggers, and urgency episodes.
Trim irritants: Cut caffeine and alcohol for 2–3 weeks; note changes.
Practice urge suppression daily: Quick pelvic squeezes + slow breathing.
Book pelvic floor PT: Ask your clinician for a referral if urgency and pelvic discomfort persist.
Discuss options: Review alpha-blockers, supplements, or herbal support like the Diuretic and Anti-inflammatory Pill with your healthcare provider.
Bottom line
If you’ve wondered, “Why can’t many patients with chronic prostatitis hold their urine?”, you’re asking the right question. The answer lies in sensitive nerves, tight muscles, and local inflammation—factors you can influence. Start with small, steady changes, consider guided therapies, and explore supportive options with your clinician. Your bladder can learn new habits, and relief is a realistic goal.
About the Creator
Health For You
Health For You! haring simple, practical wellness tips to help you thrive. Making health approachable, one story at a time!






Comments
There are no comments for this story
Be the first to respond and start the conversation.