Azoospermia Treatment
Exploring Modern Solution for Male Infertility

Azoospermia, which refers to the complete lack of sperm in a man’s semen, is a major contributor to male infertility. Affecting around 10% of infertile men globally. Treatment options for azoospermia vary depending on the underlying cause, and advancements in fertility technology, particularly in IVF, have greatly improved the chances of conception for affected individuals. This blog explores various treatment approaches, including costs and the latest innovations, like azoospermia treatment price, and the latest medical treatment of azoospermia.
A Closer Look at Azoospermia
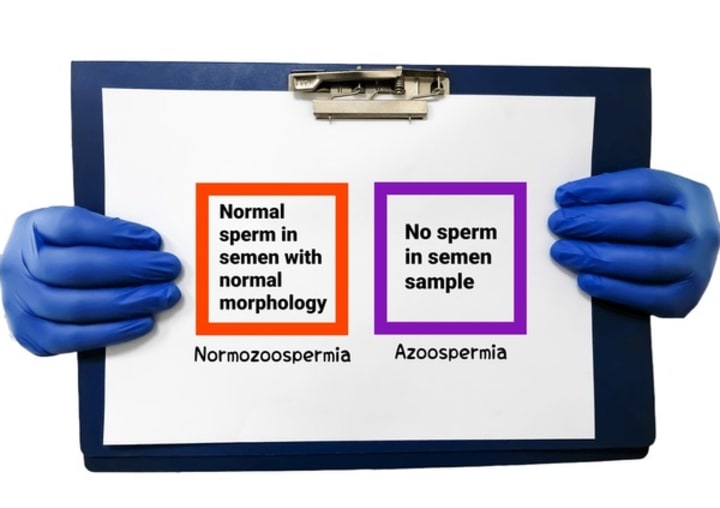
Azoospermia is generally classified into two categories: obstructive azoospermia (OA) and non-obstructive azoospermia (NOA). OA occurs due to blockages that prevent sperm from being included in the ejaculate, while NOA results from problems in sperm production. A proper diagnosis is essential to determine the right treatment plan, which could include surgery, medication, or assisted reproductive techniques such as IVF.
Azoospermia Treatment Price: What to Expect
The cost of azoospermia treatment varies based on the type of intervention required. For men diagnosed with obstructive azoospermia, surgical procedures like vasovasostomy (reversal of a vasectomy) or epididymal sperm aspiration (PESA) can restore fertility. These surgeries typically range from ₹40,000 to ₹1 lakh. Non-obstructive azoospermia treatments, however, may require more advanced approaches such as testicular sperm extraction (TESE) or micro-TESE, which could cost between ₹2 lakhs to ₹5 lakhs.
Additionally, for those opting for IVF treatments combined with intracytoplasmic sperm injection (ICSI), the overall price can escalate. IVF with ICSI costs approximately ₹1 lakh to ₹2.5 lakhs per cycle. While expensive, this remains the most effective option for men with azoospermia to achieve biological parenthood.
Most Common Medical Treatment of Azoospermia: Hormonal Therapies
For patients with non-obstructive azoospermia due to hormonal imbalances, medical treatments can help stimulate sperm production. Hormonal therapies, particularly those involving follicle-stimulating hormone (FSH) or human chorionic gonadotropin (hCG), can significantly enhance sperm count by restoring the natural hormonal balance essential for spermatogenesis.
Treatment durations vary but typically range from several months to a year, depending on the individual’s response. The price of hormone therapy can range from ₹5,000 to ₹10,000 per cycle. For men with hypogonadotropic hypogonadism (a condition that affects the production of sperm due to hormonal deficiencies), this approach has shown a 65% success rate, often enabling natural conception or boosting the chances of success with IVF and ICSI.
Heat Treatment for Azoospermia: A Controversial Approach

Heat therapy for azoospermia is an emerging, yet controversial, method that targets improving sperm production by lowering scrotal temperatures. Studies have suggested that elevated scrotal temperature, often caused by varicocele or lifestyle factors like frequent hot tub use, can impair spermatogenesis. Heat treatment for azoospermia involves cooling techniques to counteract this. Some evidence suggests that cooling the testes can increase sperm count and motility, especially in men with varicocele-associated azoospermia.
While promising, heat treatment is not universally accepted as a standard approach. It remains in the experimental phase, with more research required to validate its effectiveness. As a result, the costs for heat treatment are not as well-documented, though they are expected to be lower than surgical interventions.
Latest Treatment for Azoospermia: Innovations in IVF and Sperm Retrieval
Recent advances in fertility treatment have revolutionized the management of azoospermia. Microdissection TESE (micro-TESE) is one of the evolved treatment methods for men suffering for men with non-obstructive azoospermia. This procedure, performed under a microscope, allows for precise sperm retrieval directly from testicular tissue, even in cases of severe spermatogenic failure. Micro-TESE offers higher success rates compared to conventional methods and minimizes testicular damage.
When combined with IVF and ICSI, micro-TESE significantly increases the likelihood of conception. The latest treatment for azoospermia leverages these techniques, alongside pre-implantation genetic diagnosis (PGD) for screening embryos, ensuring that couples have a better chance of successful pregnancy while reducing the risk of transmitting genetic abnormalities associated with azoospermia.
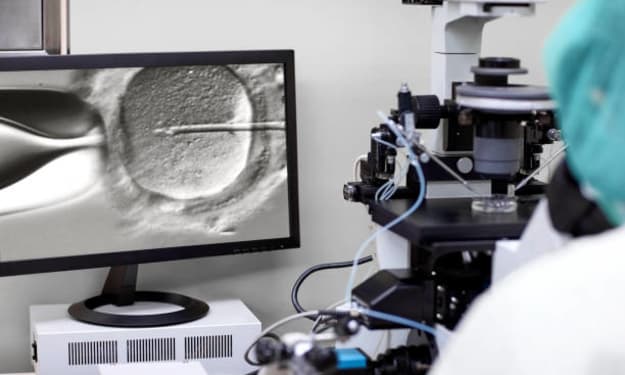
The Role of IVF in Azoospermia Treatment
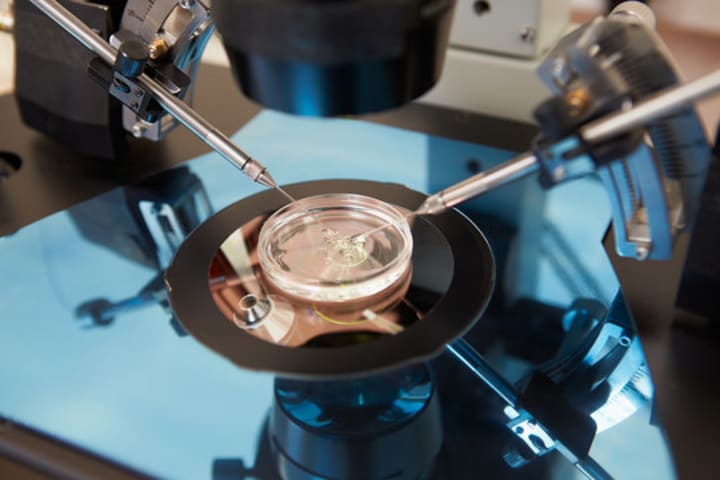
For men with azoospermia, IVF plays a central role in enabling conception. Using sperm retrieved through techniques like TESE or micro-TESE, IVF with ICSI allows the injection of a single sperm directly into an egg, bypassing the natural barriers to fertilization. This method has proven to be particularly effective for azoospermic men, as it eliminates the need for high sperm counts or motility.
Moreover, the use of donor sperm remains an option for men where sperm retrieval is unsuccessful. Although not a biological solution, donor sperm allows couples to still experience the pregnancy and childbirth process. IVF clinics often offer consultations to determine the best course of action based on the individual’s fertility diagnosis.
Conclusion
Azoospermia, once a formidable obstacle to fatherhood, now has several treatment options, thanks to medical advancements. From hormonal therapies to the latest in sperm retrieval technologies, men with azoospermia have hope. However, with the considerable costs of treatments such as IVF and surgical sperm retrieval, it’s important to discuss all available options with a fertility specialist to determine the most suitable and cost-effective plan for your unique case.
As the medical community continues to innovate, the future for azoospermic men looks fully treatable, offering them the possibility of starting their families through assisted reproductive techniques.




Comments
There are no comments for this story
Be the first to respond and start the conversation.