Latest Stories
Most recently published stories in Longevity.
A Distinct New Type of Diabetes Is Officially Recognized: A Paradigm Shift in Understanding the Disease. AI-Generated.
Diabetes, a chronic condition affecting millions worldwide, has long been categorized into two main types: Type 1, an autoimmune disorder often diagnosed in childhood, and Type 2, typically linked to lifestyle factors and insulin resistance. However, groundbreaking research has led scientists and medical professionals to officially recognize a distinct new type of diabetes, challenging traditional classifications and opening new avenues for diagnosis, treatment, and patient care. The Discovery of a New Diabetes Type The new form, sometimes referred to as Type 1.5 or LADA (Latent Autoimmune Diabetes in Adults) in previous studies, has now gained more precise recognition based on clinical and molecular evidence. Researchers found that this type does not fit neatly into the Type 1 or Type 2 categories. Unlike Type 1, it develops more slowly and often manifests in adults, while unlike Type 2, it is not primarily linked to obesity or lifestyle choices. Dr. Emily Carter, an endocrinologist involved in the research, explains, “Patients with this new diabetes type show a unique combination of autoimmune markers and insulin resistance. They often get misdiagnosed, which delays optimal treatment. Official recognition helps both patients and clinicians approach management more effectively.” Clinical Characteristics Patients with this new form of diabetes often display symptoms that overlap with both traditional types, making diagnosis complex. Common characteristics include: Gradual onset in adulthood Presence of specific autoimmune markers attacking insulin-producing cells Variable insulin resistance not linked to obesity or metabolic syndrome Slower progression to insulin dependence compared to Type 1 Because of these features, many patients were previously misdiagnosed with Type 2 diabetes, leading to treatments that may not address the underlying autoimmune component. Early identification can now allow for personalized therapy, combining lifestyle management with insulin or immune-targeted interventions. Implications for Diagnosis The recognition of a distinct diabetes type emphasizes the need for more precise diagnostic testing. Current blood glucose and HbA1c tests alone cannot differentiate this type from other forms. Instead, doctors must consider: Autoantibody testing Genetic markers Insulin production levels (C-peptide tests) With these tools, clinicians can accurately classify patients, reducing the risk of misdiagnosis and improving long-term outcomes. Treatment Strategies Treatment approaches for this newly recognized diabetes type are evolving. Because patients often experience both autoimmune damage and insulin resistance, doctors may recommend a hybrid approach: Early introduction of insulin therapy to preserve remaining pancreatic function Medications targeting insulin sensitivity Continuous monitoring to adjust therapy as disease progression varies Nutrition and lifestyle adjustments remain important, but they are often insufficient alone, particularly if autoimmune destruction of beta cells is significant. Global Health Implications The recognition of this new diabetes type has broad implications for public health. Diabetes prevalence is rising globally, and misclassification can hinder effective management and research. With a clearer understanding of this type: Epidemiological data will become more accurate Clinical trials can include patients who were previously excluded Healthcare providers can design targeted interventions to prevent complications Dr. Sanjay Mehta, a diabetes researcher, notes, “Understanding the diversity of diabetes is crucial. By recognizing this distinct type, we can reduce the risk of cardiovascular disease, kidney failure, and other complications that arise from suboptimal treatment.” Patient Awareness and Advocacy For patients, recognition means validation and better care. Many adults who struggled with inconsistent treatment outcomes now have a clear explanation for their unique experiences. Patient advocacy groups are pushing for education campaigns, ensuring that individuals and healthcare professionals alike understand this diabetes type, its symptoms, and management strategies. Future Directions The official recognition of a new diabetes type is likely just the beginning. Ongoing research aims to: Identify additional subtypes within diabetes for even more precise treatment Explore immune-modulating therapies to prevent beta-cell destruction Develop personalized medicine approaches based on genetic and molecular profiles Experts predict that the next decade will see a revolution in diabetes care, driven by these insights and the increasing emphasis on individualized treatment. Conclusion The recognition of a distinct new type of diabetes represents a major milestone in medical science. It highlights the complexity of the disease and challenges long-standing assumptions. With improved diagnosis, targeted therapies, and patient education, this breakthrough promises better outcomes for millions worldwide. This development also underscores the importance of ongoing research and awareness in understanding chronic diseases. As healthcare systems adapt to these insights, patients can look forward to more precise, effective, and personalized care, moving closer to a future where diabetes management is tailored to the individual rather than a one-size-fits-all approach.
By Fiaz Ahmed Brohi24 days ago in Longevity
4 Daily Rules That Reduced My Stress
I didn’t realize how stressed I was until my body forced me to stop. One morning, I woke up exhausted before the day even began. My mind was racing, my chest felt tight, and the smallest tasks felt overwhelming. From the outside, my life looked normal—work, responsibilities, routines—but inside, I was constantly tense. I was always rushing, always thinking, always worrying. That’s when I knew something had to change.
By Fazal Hadi24 days ago in Longevity
How To Lose Christmas Weight And Feel Lighter Before New Year's Eve
The week after Christmas often comes with a familiar feeling - a mix of food coma, sluggishness, and the quiet worry of fitting into your New Year's Eve outfit. The good news? You don't need extreme detoxes or punishing workouts to bounce back. Consultant nutritionist Rupali Datta recommends five days of smart, home-style eating to reset your system and bring your energy back. Think simple meals, gentle movement, and the realisation that your body responds beautifully when you give it a little attention. You don't need perfection - just momentum. With small tweaks in your kitchen and a return to lighter plates, you can shed the post-festive bloat, feel fresher, and step into the New Year with confidence
By Good health to everyone24 days ago in Longevity
The Simplest Way to Lose Belly Fat
I'm going to talk about how to burn belly fat step-by-step. There's really three basic sections: the basics of what to do, things to add to speed up weight loss, and things to avoid to speed up weight loss. Okay, so let's talk about the basics first—and some of this might be just repetitive, but if you've never seen an article from me, this will be very helpful.
By Edward Smith24 days ago in Longevity
Cardio Is Great - But Walking Is All You Really Need
Cardio has become synonymous with suffering. Sweat-drenched shirts. Burning lungs. Heart pounding out of your chest. The idea that if it doesn't hurt, it doesn't count has been rampaging as the evergreen message.
By Destiny S. Harris24 days ago in Longevity
3 Mental Habits That Saved Me During My Lowest Phase
I didn’t hit rock bottom in one dramatic moment. It happened slowly. Days blurred together. Nights felt endless. I smiled in front of people and collapsed the moment I was alone. I wasn’t lazy, weak, or broken—but I felt like all three. Every plan I made felt pointless. Every effort felt invisible. And the scariest part was this: I started believing that this version of my life was permanent.
By Fazal Hadi25 days ago in Longevity
Living With Diabetes as We Age
Diabetes is one of those conditions that quietly but deeply reshapes daily life. When it appears later in life, it can feel like an additional burden at a stage when many people already feel physically and emotionally more vulnerable. For older adults, diabetes is often experienced not only as a medical diagnosis, but as a loss of freedom, a source of worry, or even a form of injustice. These feelings are normal. Diabetes does not affect only the body; it also touches self-image, daily routines, confidence, and the way one imagines the future.
By Bubble Chill Media 25 days ago in Longevity
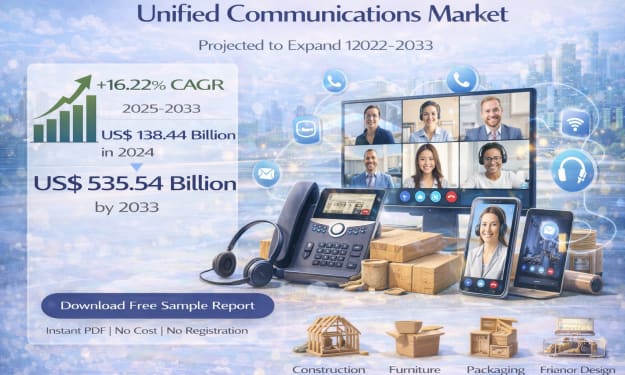
Unified Communications Market Size and Forecast 2025. AI-Generated.
Unified Communications Market Snapshot According to Renub Research, the Unified Communications Market is projected to expand from US$ 138.44 billion in 2024 to US$ 535.54 billion by 2033, growing at a robust CAGR of 16.22% from 2025 to 2033.
By Aaina Oberoi25 days ago in Longevity
Australia Radiofrequency Ablation Device Market Size and Forecast 2025–2033. AI-Generated.
Market Snapshot (As per Renub Research) The Australia Radiofrequency Ablation (RFA) Device Market is on a strong growth trajectory and is expected to reach US$ 176.63 million by 2033, up from US$ 84.41 million in 2024, expanding at a CAGR of 8.55% from 2025 to 2033.
By Aaina Oberoi25 days ago in Longevity
This Common Blood Pressure Drug Boosts Lifespan and Slows Aging in Animals. AI-Generated.
In the search for longer, healthier lives, scientists often look in unexpected places. One such place is the medicine cabinet. Recent research suggests that a widely used blood pressure drug may do more than control hypertension—it could extend lifespan and slow biological aging, at least in animal models. While the findings are still far from proving a human anti-aging cure, they offer intriguing clues about how existing medications might influence the aging process. A Surprising Discovery in a Familiar Drug The drug at the center of this research belongs to a class of medications commonly prescribed to millions of people worldwide for high blood pressure and heart disease. These drugs have been used safely for decades, making them especially interesting to scientists exploring “drug repurposing”—the idea that existing medicines might have benefits beyond their original purpose. In laboratory studies involving animals such as mice and worms, researchers observed that animals treated with this blood pressure medication lived longer and showed signs of delayed aging. These weren’t just marginal improvements. In some cases, lifespan increased significantly, and the animals remained healthier and more active later in life compared to untreated counterparts. How Can a Blood Pressure Drug Affect Aging? Aging is not controlled by a single switch. It is influenced by complex biological pathways involving inflammation, cellular stress, metabolism, and damage repair. The blood pressure drug studied appears to interact with several of these pathways. One key factor is cellular stress response. As organisms age, cells become less efficient at managing stress caused by toxins, inflammation, and metabolic imbalance. The drug seems to enhance the body’s natural defense systems, helping cells cope better with stress and reducing long-term damage. Another important mechanism involves mTOR and insulin signaling pathways, which play a major role in aging and longevity. These pathways regulate how cells grow, divide, and use energy. Overactivity in these systems has been linked to faster aging. Researchers believe the drug subtly dampens these signals, mimicking the effects of calorie restriction—one of the most well-documented ways to extend lifespan in animals. Healthspan Matters More Than Lifespan One of the most encouraging aspects of the findings is that the animals didn’t just live longer—they lived better. Scientists use the term “healthspan” to describe the period of life spent in good health, free from chronic disease and disability. In the studies, treated animals showed: Better mobility at older ages Improved cardiovascular and metabolic health Lower levels of age-related inflammation Delayed onset of age-associated decline This distinction is crucial. Extending life without preserving quality would be far less meaningful. The results suggest the drug may help compress aging, allowing animals to stay healthier for longer and decline more gradually. What Does This Mean for Humans? Despite the excitement, researchers are careful to emphasize that animal studies do not guarantee human results. Many treatments that work in mice fail to produce the same effects in people. Human aging is more complex, influenced by genetics, environment, lifestyle, and social factors. However, the fact that this drug is already approved and widely prescribed gives scientists a head start. Its safety profile is well understood, which lowers barriers for future clinical trials. Some researchers are now calling for long-term human studies to examine whether people taking this medication experience slower biological aging or reduced risk of age-related diseases. It’s also important to note that this drug should not be taken solely for longevity purposes without medical supervision. Blood pressure medications can have side effects and may not be appropriate for individuals without cardiovascular conditions. A Growing Trend: Repurposing Existing Drugs This research fits into a broader trend in longevity science. Instead of developing entirely new anti-aging drugs, scientists are re-examining familiar medications such as metformin, rapamycin, and now blood pressure drugs for their potential lifespan benefits. The appeal is clear: repurposed drugs are cheaper, faster to test, and safer than experimental compounds. If even a fraction of their benefits translate to humans, they could have a profound impact on public health, especially in aging populations. The Bigger Picture of Aging Research While no pill can stop aging entirely, studies like this shift how we think about it. Aging is increasingly viewed not as an inevitable decline, but as a modifiable biological process. Small interventions—pharmaceutical, dietary, or lifestyle-based—may collectively make a significant difference. For now, the best evidence-backed strategies for healthy aging remain regular exercise, balanced nutrition, stress management, and medical care. Still, the idea that a common blood pressure drug could one day join that list is both fascinating and hopeful. Final Thoughts The discovery that a routine blood pressure medication can extend lifespan and slow aging in animals highlights the untapped potential hidden in everyday drugs. While human confirmation is still needed, the findings open exciting doors for aging research and reinforce the idea that the future of longevity may already be sitting on pharmacy shelves—waiting to be fully understood.
By Fiaz Ahmed Brohi25 days ago in Longevity