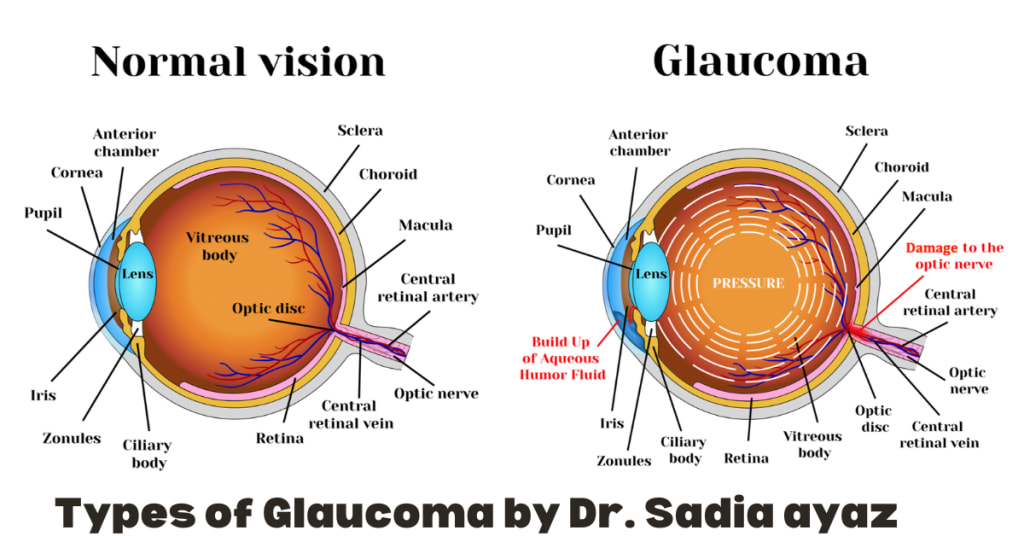
Types of Glaucoma
Glaucoma is an irreversible blinding disease of all age groups. The prognosis of glaucoma is defined on the basis of the different types of glaucoma. The early detection and timely commencement of treatment is the key to a better prognosis so that a patient will not become blind in his lifetime.
In glaucoma the optic nerve is damaged along with a reduction in the visual fields in which raised intraocular pressure is the main risk factor. One or both eyes are involved, depending upon the cause. The rise in intraocular pressure will directly/ mechanically or indirectly damage the optic nerve, responsible for signaling the image to the brain.
The majority of the patients develop no symptoms in the early stages. Patients having positive family and risk factors should pay a regular visit to the health professional.
The management plan and signs and symptoms depend upon the type of glaucoma.
Are There Different Types of Glaucoma?
Primary Congenital Glaucoma:
Glaucoma may begin in the early stages of life or even in the intrauterine period.Primary Congenital Glaucoma Depending upon the time of onset, it can be classified as under True congenital glaucoma in which intraocular pressure is raised during intrauterine period.
Infantile glaucoma manifest during first 3 years of life.
Juvenile glaucoma in which IOP rises between 3 to 15 years of age.
Primary congenital glaucoma is not associated with any other systemic complications. The pathology lies in trabeculodysgenises. Secondary infantile glaucoma is associated with other conditions such as retinoblastoma, uveitis, aniridia, etc.
Presentation: Primary congenital glaucoma manifest as corneal haze with watering, Haab’s stria on the Descemet membrane, enlarged corneal diameter, raised intraocular pressure, changes in the optic disc, and corneal vascularization. The evaluation is done under general anesthesia that includes measurement of corneal diameter, IOP, refraction, and optic disc.
Treatment options: Treatment of congenital glaucoma depends upon the clarity of cornea. If cornea is clear, goniotomy is performed, and if cornea is hazy trabeculotomy or trabeculectomy is done.
Primary Open Angle Glaucoma:
the commonest cause of glaucoma. In POAG there is no contact between iris and trabeculae, hence the angels are open. The main pathology lies when particles of Different types of glaucoma different types, depending upon the type of glaucoma blocks the trabecular meshwork. The outflow process of aqueous humor is reduced leading to raised intraocular pressure.
Secondary Open Angle Glaucoma:
The following types of secondary open-angle glaucoma can be defined.
What is pseudoexfoliation syndrome?
Pseudo exfoliative glaucoma:
In pseudoexfoliative glaucoma, the amyloid-like extracellular substance is deposited in various tissues of the body including the eye. the material will get deposited in the trabecular meshwork and obstruct the outflow pathway of aqueous humor.
Clinical Features Include:
Pseudo exfoliative material deposition on the margins of pupil Anterior lens capsule shows deposition of pseudo exfoliation material in a disc shape pattern
Treatment options:
Treatment usually starts with topical medications depending upon the overall health of the patient. Other treatment option includes laser trabeculoplasty and filtration surgery with shunts.
Pigment Dispersion Glaucoma:
In PDG pigments from the posterior surface of the iris are released.Pigment Dispersion Glaucoma
There is deposition of pigments in the anterior chamber and in endothelium and lens. It is common in myopes. The incidence is more in young males.
Pathogenesis:
There is excessive backward bowing of the iris, resulting in constant rubbing again the zonules and hence the release of pigments. It can be precipitated with extensive movements, such as during exercise.
Clinical features:
Kruk Enberg spindles on corneal endothelium
Aqueous flare in anterior chamber
Spoke like trans illumination defects in mid iris.
Sampaolesi line anterior to Schwalbe line.
Zentmyer ring around the equator, at the region of zonule insertion.
Posterior segment may show glaucomatous optic neuropathy and peripheral retinal degeneration.
Treatment options:
Lifestyle modification: avoiding activities such as jogging and running. In case exercise is must, pilocarpine eye drops should be used prophylactically.
Medical treatment: medical treatment is the same as other types of open angle glaucoma.
Neovascular Glaucoma:
Pathogenesis:
In neovascular glaucoma, the common pathology is related to hypoxia of the retinal tissue which leads to the production of angiogenic factors. The factors induce both retinal and anterior segment neovascularization.
Causes:
These includes
Ischemic central retinal vein occlusion
Diabetes mellites
Arterial retinal vascular disease
Intraocular tumors
Retinal detachment
Clinical features:
Corneal edema
Raised intraocular pressure
Aqueous chamber flare with posterior synechiae.
Neo vessels on the surface and towards the angle.
Cataract
Glaucomatous optic neuropathy
Treatment options:
Treatment of neovascular glaucoma depends upon the cause of neovascularization
Medical treatment: it depends upon the visual potential of the patient. When there is no visual potential, atropine along with steroids are adequate
Pan retinal photocoagulation:
Intraocular VEGF inhibitors:
Ciliary body ablation:
Filtration surgery:
What Is Uveitis Glaucoma ?
Inflammatory Glaucoma
In this type of glaucoma, the raised intraocular pressure is secondary to intraocular inflammation. The cause may include any inflammatory process going on in the eye for example in hyphema cases, there is the attachment of the iris to the trabeculum, as a result, the pupil may get completely blocked. In other types such as uveitis in the anterior chamber, the cause may be trabeculitis or trabecular meshwork obstruction by the inflammatory substance.
Treatment options:
Treatment depends upon the cause.
In pupillary block cases laser iridotomy should be performed, to reestablish the communication between anterior and posterior chamber.
In uveitic cases steroids and cycloplegic eye drops should be used.
In refractory cases, trabeculectomy with mitomycin C or glaucoma valves should be employed.
What Is Phacomorphic Glaucoma ?
Lens Related Glaucoma:
This type of glaucoma can be divided into the following types
Phacolytic Glaucoma:
This is a type of open-angle glaucoma due to a hyper mature cataract. The trabecular meshwork is blocked with high molecular proteins released through the intact capsule of the maturing lens.
It is different from phacoanaphylactic glaucoma, in which there is an immune reaction to the lens proteins with a compromised lens capsule.
Treatment:
Treatment involves medically controlled IOP and later on wash out of the proteaceous material from the anterior chamber.
Phacomorphic Glaucoma:
Phacomorphic glaucoma is secondary angle-closure glaucoma, in this type of glaucoma, the intumescent cataract associated with slacken zonules is pulled anteriorly to block the pupil and cause iris bombe.
Treatment:
The definitive treatment is cataract surgery.
What Is Malignant Glaucoma ?
Angle-Closure Glaucoma:
In angle-closure glaucoma, the trabecular meshwork is blocked by the peripheralDifferent types of glaucoma iris, (iridotrabecular contact, ITC). It can be primary, due to anatomically exposed eye or secondary, due to another ocular or systemic condition.
Classification:
Primary angle-closure suspect:
Gonioscopy show ITC in 3 or more quadrants but no peripheral anterior synechiae (PAS).
Normal IOP, optic disc and visual fields.
Primary angle closure:
Gonioscopy show ITC in 3 or more quadrants.
Raised IOP and PAS
Normal optic disc and visual fields.
Primary angle closure glaucoma:
ITC in 3 or more quadrants
Raised IOP
Glaucomatous optic disc changes
Visual field defects
Causes of angle-closure: These includes
Relative pupillary block and anterior bowing of peripheral iris
Non pupillary block with plateau iris
Lens induced closure, as in phacomorphic glaucoma
Retro lenticular glaucoma, as in malignant glaucoma, caused in postoperative trabeculectomy surgery.
Risk factors:
Age: the average age at presentation is 60 years
Race: it is more common in Far Eastern and Indian Asians.
Gender: females are more commonly affected than males.
Refraction: it is typically common in hypermetropic.
Axial length: short eyes and nanophthalmos have short axial length and are particularly prone to angle closure.
Symptoms:
Most of the patients have chronically raised IOP without any symptoms. Common presentation is decreased vision, haloes, blurring, redness, periocular pain, and headache. Others include emotional stress, semi-prone position, cold or flu remedies, using topiramate and other sulfa drugs.
Signs:
Reduced visual acuity, 6/60 to HM.
Raised IOP of 50-100 mmHg
Corneal edema
Shallow anterior chamber
Unreactive mid dilated pupil
Which Glaucoma Is Considered a Medical Emergency ?
Acute angle closure is a medical emergency and steps should be taken to immediately rescue the patient from the prevailing condition.
The patient should assume prone position
Oral and intravenous acetazolamide given, according to the measure IOP.
In resistant case intravenous mannitol 20% should be administered.
Early iridotomy or iridoplasty should be done once the corneal edema clears.
Subsequent management includes starting alpha blockers, beta blockers, steroid and oral acetazolamide.
Bilateral laser iridotomy is performed once the cornea clears and IOP is normalized.
What Is The Difference Between Open- Angle and Closed- Angle Glaucoma?
In open-angle glaucoma, the trabecular meshwork is blocked by substances such as pigments, inflammatory material, pseudoexfoliation while in angle-closure glaucoma, there is iridotrabecular contact by the peripheral iris or the lens. Angle-closure glaucoma can present as an acute emergency while the same is not true for open-angle glaucoma. for more click here
About the Creator
sadia ayaz
My name is Dr. Sadia Ayaz and I am an ophthalmologist and eye surgeon. My medical degree is from Pakistan, I have done FCPS-1 / IMM from the College of Physicians and Surgeons Pakistan.




Comments
There are no comments for this story
Be the first to respond and start the conversation.