The Future of Biomedical Innovation: Organ-on-Chip Technology
Pioneering a New Era in Human Health Research and Precision Medicine
In recent years, the biomedical landscape has undergone a profound transformation with the emergence of micro-engineered platforms that replicate the functional units of human organs. Among these innovations, Organ-on-Chip technology stands out as a groundbreaking tool poised to redefine how we study diseases, develop drugs, and personalize medical treatments. Combining advances in tissue engineering, microfluidics, and cellular biology, this technology offers a highly sophisticated alternative to conventional animal testing and 2D cell cultures.
What Is Organ-on-Chip?
Organ-on-Chip is a microfluidic device — roughly the size of a USB stick — lined with living human cells and designed to mimic the key physiological functions of specific organs such as the heart, lung, liver, kidney, or brain. Unlike traditional cell culture models, which grow cells on flat petri dishes, these chips recreate the three-dimensional microenvironment of human tissues. The chips integrate tiny channels through which fluids can flow, simulating blood circulation and delivering nutrients and drugs in a controlled manner.
What makes this technology unique is its ability to mimic the mechanical forces and biochemical signaling present in human organs. For example, a lung-on-chip can simulate breathing motions, while a heart-on-chip can beat rhythmically. These dynamic and interactive systems bring unprecedented physiological relevance to laboratory experiments.
The Limitations of Traditional Preclinical Models
For decades, drug development has relied heavily on 2D cell cultures and animal testing. While these methods have provided critical insights, they suffer from major limitations:
1. Lack of Human Relevance: Animal physiology often differs significantly from human biology. Many drugs that appear safe and effective in animals fail during human clinical trials.
2. Simplistic Models: 2D cultures lack the complexity of real tissues, ignoring important interactions between different cell types.
3. Ethical Concerns: Animal testing raises ethical questions and faces increasing regulatory scrutiny.
4. High Costs and Time: Drug development using traditional methods is time-consuming and expensive, with a success rate of less than 10% for compounds entering clinical trials.
Organ-on-Chip systems address many of these issues by offering a more human-relevant platform for testing and discovery.
How Organ-on-Chip Technology Works
These devices are typically fabricated using soft, flexible polymers like polydimethylsiloxane (PDMS). The process involves several key components:
• Microfluidic Channels: These mimic blood vessels and allow precise control of fluid flow.
• Living Cells: Human-derived cells are cultured within the chip to replicate organ-specific functions.
• Sensors and Actuators: Integrated sensors monitor biological responses such as pH, oxygen levels, and electrical activity.
• Mechanical Stimulation: Some chips incorporate mechanical forces — like stretching or pulsation — to emulate natural organ motion.
The result is a miniaturized, functional organ model that behaves remarkably like its counterpart in the human body. This makes it ideal for studying disease mechanisms, drug metabolism, and toxicity.
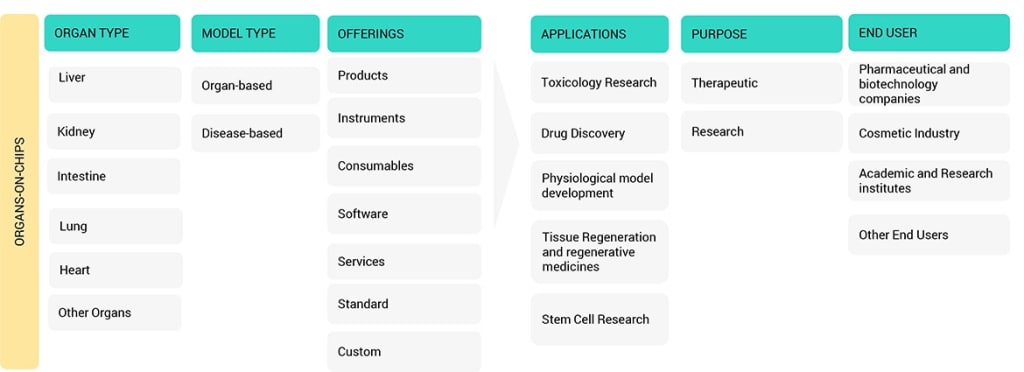
Applications Across the Biomedical Spectrum
1. Drug Development and Toxicity Testing
One of the most promising applications of Organ-on-Chip technology is in pharmaceutical research. Before drugs reach clinical trials, they must undergo rigorous safety testing. Traditional models often fail to predict human responses accurately. Organ-on-Chip platforms can bridge this gap by providing more predictive, cost-effective, and ethical testing environments.
For example:
• Liver-on-Chip can model drug metabolism and identify potential liver toxicity early in the development process.
• Heart-on-Chip can assess cardiotoxicity risks, which are a leading cause of drug withdrawals from the market.
2. Disease Modeling
Organ-on-Chip allows researchers to recreate disease states in a controlled lab environment. By using patient-derived cells, scientists can model complex conditions like cancer, fibrosis, neurodegenerative diseases, or infectious diseases. This enables a deeper understanding of pathophysiology and the identification of new therapeutic targets.
3. Personalized Medicine
Because Organ-on-Chip devices can be built using cells from individual patients, they hold tremendous potential for personalized treatment strategies. For instance, a chip derived from a cancer patient’s tumor cells could be used to test different drug regimens and select the most effective therapy — all before administering the drug to the patient.
4. Regenerative Medicine and Organ Transplant Research
Researchers are exploring how Organ-on-Chip systems can help develop tissue regeneration strategies and evaluate organ compatibility before transplantation. This could reduce transplant rejection rates and improve patient outcomes.
Integration with Emerging Technologies
Organ-on-Chip is not an isolated technology; it thrives at the intersection of multiple cutting-edge fields:
• Artificial intelligence and Machine Learning: AI algorithms can analyze complex data from chips to predict clinical outcomes more accurately.
• 3D bioprinting: This can be used to precisely position cells within chips, enhancing tissue structure realism.
• Organoid Integration: Combining organoids with Organ-on-Chip devices creates more physiologically relevant and complex models, sometimes called “Body-on-a-Chip” systems.
• Multi-Organ Systems: By linking several chips, researchers can study organ-organ interactions, drug metabolism, and systemic effects within a single platform.
Challenges and Barriers to Adoption
Despite its promise, Organ-on-Chip technology faces certain challenges:
• Technical Complexity: Fabricating chips with precise microenvironments requires advanced engineering and expertise.
• Scalability: Standardizing and mass-producing chips remains a hurdle for widespread adoption.
• Regulatory Framework: There is still a need for clear guidelines to support regulatory acceptance in drug approval processes.
• Data Interpretation: The massive amount of data generated requires sophisticated analytical tools and expertise.
However, ongoing research and cross-disciplinary collaborations are addressing these issues, bringing the technology closer to mainstream adoption.
The Road Ahead
The future of Organ-on-Chip technology looks exceptionally bright. As it continues to evolve, it is expected to:
• Reduce drug development costs and timelines by improving preclinical prediction accuracy.
• Accelerate the discovery of new therapies through better disease modeling.
• Enable truly personalized medicine, tailoring treatments to individual patients.
• Decrease reliance on animal testing, aligning with global ethical and regulatory shifts.
Moreover, as multi-organ systems become more sophisticated, the ultimate goal of creating a “human-on-a-chip” platform — capable of mimicking the entire body’s physiology — is becoming increasingly achievable.
Conclusion
Organ-on-Chip represents one of the most transformative innovations in modern biomedicine. By combining engineering precision with biological complexity, it provides an unparalleled window into human physiology and disease. Its applications span from pharmaceutical development to personalized healthcare, making it a cornerstone of next-generation medical research.
As technology matures and regulatory frameworks adapt, Organ-on-Chip has the potential to revolutionize how we develop drugs, understand diseases, and deliver patient care — paving the way for a safer, faster, and more effective future in medicine.





Comments
There are no comments for this story
Be the first to respond and start the conversation.