Revenue cycle management (RCM): What healthcare businesses need to know
Revenue Cycle Management in Healthcare
Introduction to Revenue Cycle Management (RCM)
In the fast-paced world of healthcare, where every second counts and patient care is paramount, understanding the intricacies of revenue cycle management (RCM) can set your business apart. Revenue cycle management isn’t just a buzzword; it’s an essential practice that determines how efficiently a healthcare organization operates financially. From scheduling appointments to billing insurance companies, each step in the RCM process impacts not only cash flow but also patient satisfaction.
For healthcare businesses navigating this complex landscape, grasping the fundamentals of RCM is crucial. It’s about more than just collecting payments; it's about creating a streamlined approach that enhances operational efficiency while ensuring patients receive top-notch service. Whether you are part of a large hospital system or running a small clinic, mastering healthcare revenue cycle management can lead to improved financial health and sustainable growth for your practice.
Let’s dive into what makes RCM so important for healthcare organizations today and explore how implementing effective strategies can transform your bottom line and elevate patient experiences like never before.
The Importance of RCM in Healthcare Businesses
Revenue Cycle Management (RCM) is a cornerstone of financial health in healthcare businesses. It streamlines the entire process from patient registration to final payment, ensuring efficient revenue flow.
Effective RCM significantly reduces billing errors and claim denials. This not only enhances cash flow but also improves patient satisfaction. When patients receive clear information about their costs, they are more likely to engage with services.
Moreover, RCM allows healthcare providers to focus on what matters most—patient care. By outsourcing or optimizing these processes, organizations can allocate resources more effectively.
Additionally, strong RCM practices help compliance with ever-changing regulations. Adapting quickly to new rules protects against costly penalties and audits. Investing in robust revenue cycle management services leads to sustainable growth for healthcare businesses while fostering trust within the community they serve.
Key Components of RCM
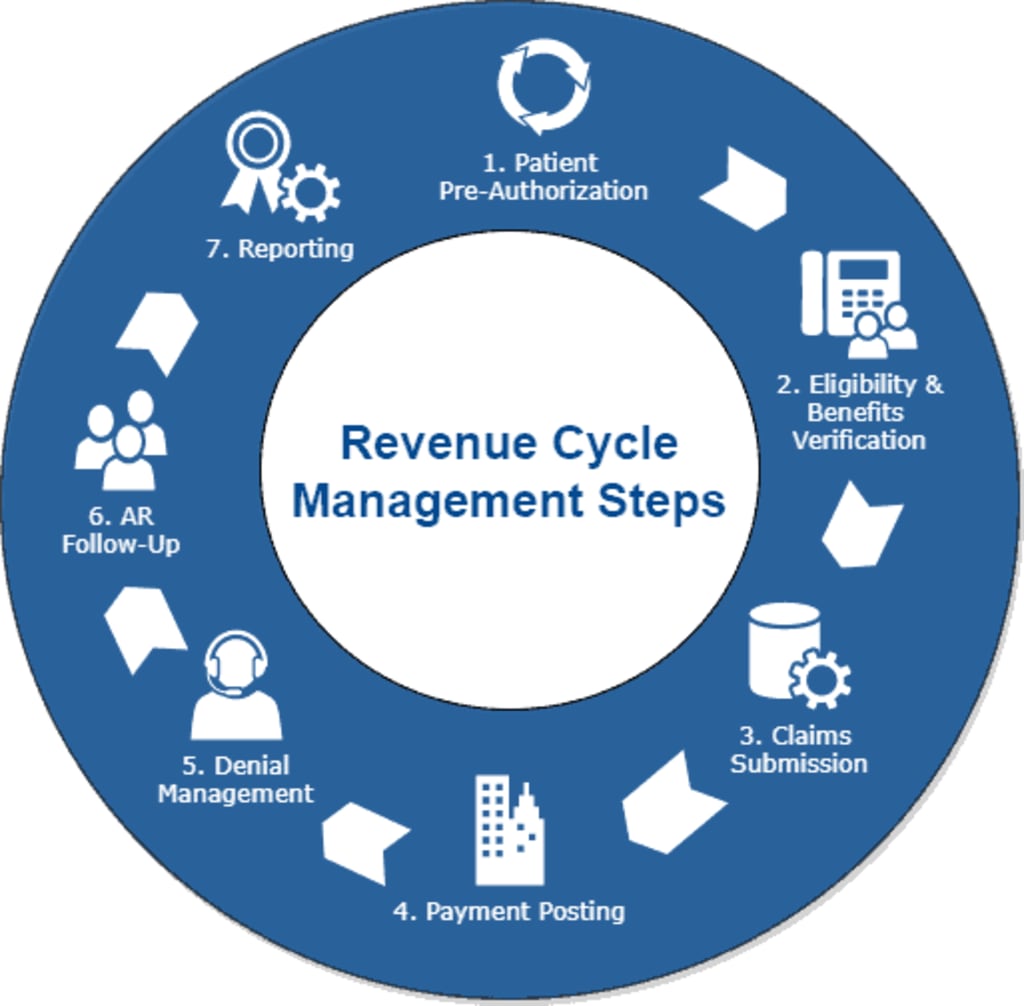
Revenue cycle management (RCM) comprises several key components that ensure a smooth flow from patient registration to final payment. First, patient access is crucial. This includes appointment scheduling and insurance verification, laying the foundation for accurate billing.
Next comes charge capture. This step involves documenting all services provided during a visit or procedure, ensuring nothing is missed in the billing process. Claims submission follows closely behind. Here, healthcare providers submit claims to insurers for reimbursement based on the captured charges.
Payment posting integrates payments received into the system, allowing organizations to track outstanding balances effectively. Accounts receivable management handles follow-up with patients and payers on unpaid claims or balances. Each component plays a vital role in maintaining cash flow and operational efficiency within healthcare revenue cycle management systems.
Common Challenges in RCM and How to Overcome Them
Healthcare revenue cycle management often faces several challenges. One major issue is billing errors, which can lead to delayed payments and frustrated patients. Ensuring accurate coding and thorough documentation is essential for minimizing these mistakes. Another common challenge arises from the complexity of insurance claims. Navigating different payer requirements can be overwhelming. Regular training for staff on changing regulations helps streamline this process.
Staffing shortages also pose a significant hurdle in RCM. A lack of skilled professionals may slow down operations and affect revenue flow. Partnering with reputable revenue cycle management companies can alleviate this burden by providing access to trained experts.
Additionally, patient engagement plays a critical role in timely collections. Many patients struggle with understanding their bills or payment options. Clear communication strategies and educational resources can enhance patient awareness, leading to improved cash flow for healthcare organizations.
Best Practices for Successful RCM Implementation
Implementing healthcare revenue cycle management successfully requires careful planning and execution. Start by assembling a dedicated team that understands the intricacies of RCM. This group should include professionals from finance, billing, and clinical services to ensure all perspectives are represented. Next, invest in training for your staff. Familiarity with systems and processes increases efficiency and reduces errors. Regular workshops can keep everyone updated on best practices.
Choose the right technology solutions tailored to your organization’s needs. The integration of user-friendly software can streamline tasks like patient scheduling, billing, and collections. Regularly review performance metrics to identify areas needing improvement. Tracking key indicators helps in making informed decisions quickly.
Maintain open communication with all stakeholders involved in the process—this includes patients as well as internal teams—to create a seamless experience throughout the revenue cycle.
Emerging Technologies and Trends in RCM
he landscape of healthcare revenue cycle management is rapidly evolving, driven by technology. Artificial Intelligence (AI) and machine learning are transforming how data is processed. These innovations help in predicting payment trends and identifying potential billing errors before they happen.
Blockchain technology is also making waves in RCM. By providing transparent and secure transactions, it enhances trust between providers and payers. This could lead to fewer disputes over claims. Telehealth has become a staple for many practices, which adds complexity to the revenue cycle but also creates opportunities for new workflows that can streamline processes.
Robotic Process Automation (RPA) reduces manual tasks, allowing staff to focus on more strategic activities instead of repetitive data entry or claim follow-ups. As these technologies continue to emerge, they promise efficiency gains that every healthcare business should consider integrating into their operations.
Conclusion: Why RCM is Crucial for the Success of Healthcare Businesses
Healthcare revenue cycle management is not just a backend process; it’s the backbone of financial health for medical practices and hospitals. Effective RCM ensures that healthcare providers receive timely payments, which in turn allows them to focus on patient care.
The complexities of billing, insurance claims, and patient payments can easily overwhelm staff if not managed properly. Revenue cycle management services streamline these processes, reducing administrative burdens. When implemented effectively by top healthcare revenue cycle management companies, RCM enhances operational efficiency and boosts profitability. This creates a sustainable environment where healthcare businesses can thrive amidst changing regulations and industry demands.
Investing in robust RCM strategies ultimately translates to improved cash flow and better service delivery. For healthcare organizations aiming for long-term success, mastering their revenue cycles is non-negotiable. f you need any further details about healthcare RCM, you can click here.
About the Creator
Luke James
Content Strategist






Comments (1)
Very good to know! Great work