Healthcare Payer Analytics Ultimately Benefits the Providers, Patients, and the Payers
Healthcare Payer Analytics
Insurance payers can be said to form the cornerstone of the American healthcare industry. The amount of money spent on healthcare in America crossed $3.5 trillion, which is more than the economy of all but four countries. Most of the money for that spending comes from the insurance payers. So it becomes necessary for payers to implement software for healthcare payer analytics.
Analyzing business data helps the company management improve operational efficiency. Healthcare payer analytics solutions assess historic and financial data of the insurance company to reveal important patterns about their provider network, members, health plans, reimbursements, claims, and so forth. Based on this information, the company can make informed decisions to serve its stakeholders better. This might involve hiring more staff to process claims faster, modifying health plans for optimizing expenditure, onboarding doctors whose care delivery aligns with payer goals, and so on.
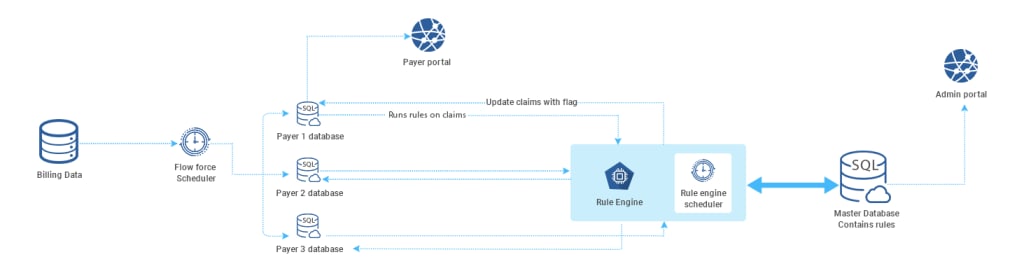
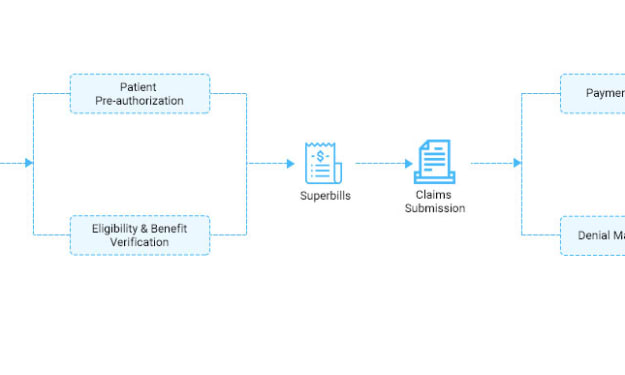
Among the most important aspects of a payer’s operations is the processing of claims. Claims might come from one of the many providers they would have tied up with. Moreover, each of the claims is bound to be different since the patients would have different diseases and varying health plans. So, assessing the data from the history of claims enables healthcare payer analytics systems to highlight important insights that help them understand the industry better.
It is no secret that American healthcare spending has been skyrocketing. The recent pandemic exacerbated the problems in the system. In light of this, there has been a growing push among clinicians, payers, and people for a more value-based model of reimbursements. This model pays physicians based on the clinical outcomes they are able to achieve for their patients. It has been widely touted to be an effective way of controlling the burgeoning costs of American healthcare and making it work for the average person.
A shift over to a value-based model requires extensive changes in the industry. The very nature of claims might need to be changed and the kind of medical documentation and coding required would have to be adjusted for a value-based care model. In light of this, it is imperative for payers to leverage the power of health care payer analytics and identify pain points in the industry to help speed up the shift over to the value-based model.
One of the exciting possibilities of healthcare provider analytics is the power to assess the health situation of entire populations or even parts. It has been accepted among providers as well as medical researchers that certain ethnic groups are more vulnerable to certain diseases than others. In other words, there is variation in genetic predisposition for diseases among people of different ethnicities. This insight goes a long way in helping both payers and providers to serve the people better. Insurance payers would know which person might need what kind of coverage based on historical data derived from analyzing payer information.
To sum it up, healthcare payer analytics would help maximize the efficiency and productivity of operations and benefit all stakeholders involved.
The most promising aspect of healthcare payer analytics is that it may have a role to play in making a switch from the traditional fee-for-service model to a value-based reimbursement model. It’s no secret that healthcare in the United States is the most expensive compared to anywhere else in the world. American spending on healthcare is estimated to be somewhere near $4 trillion! That is more than the entire economies of all three countries. One big reason for that is the existing fee-for-service model of payments.
As the name indicates, the fee-for-service model pays providers based on the quantity of service provided - as in the number of tests, scans, and treatments. Needless to point out, this incentivizes providers to keep piling on the tests, scans, treatments and even extend the hospitalizations. On the other hand, a value-based payment system pays doctors on the medical outcomes of the patients. In other words, the quality of care determines the reimbursement for the provider, as opposed to quantity.
Analyzing a provider’s claims highlights details about bundled payments and risks. Such information enables payers to make informed decisions about providers’ practices and also helps healthcare organizations partner with high-value providers who are more likely to align with organizational goals and help improve the quality of care.




Comments
There are no comments for this story
Be the first to respond and start the conversation.