"How the NHS Is Leading the Global Fight Against Melanoma with Custom Cancer Vaccines"
"Through fast-tracked trials and cutting-edge immunotherapy, the NHS is transforming melanoma care with tailored, needle-free cancer vaccines."

NHS England is rolling out a pioneering trial of a cancer vaccine for melanoma under its wider Cancer Vaccine Launch Pad (CVLP) initiative. This comes after earlier success with personalized bowel cancer vaccines and now extends to patients battling advanced skin cancer. The revolutionary, needle-free mRNA vaccines, tailor-made to every patient, are a new spark of hope and could transform cancer treatment, being a huge step forward in combating this virulent disease.
Why This Trial Is a Game Changer
The NHS is now offering a groundbreaking cancer treatment called Capivastib, which offers fresh hope by slowing the progression of breast cancer that can't be cured. Additionally, the NHS's new cancer vaccine launch pad is speeding up access to personalized mRNA cancer vaccine trials. These vaccines, unlike conventional treatments, teach healthy tissue to guide the immune system in accurately attacking cancer cells. This marks a significant shift towards precision therapy and positions the UK at the forefront of cutting-edge cancer care worldwide.

Needle-Free, Personalized, and Fast-Tracked
England's NHS is a revolution in the treatment of melanoma using a needle-free, sharp, customized vaccine test of Scandal. This novel, the first vaccine, is specially prepared from each patient's unique tumor gene code to educate the immune system to completely target and eliminate cancer cells. As part of the cancer vaccine launch pad initiative, the program will treat more than 10,000 patients by the year 2030. It is the largest deployment of individual cancer immunotherapy in a national health system, which sets an international standard.
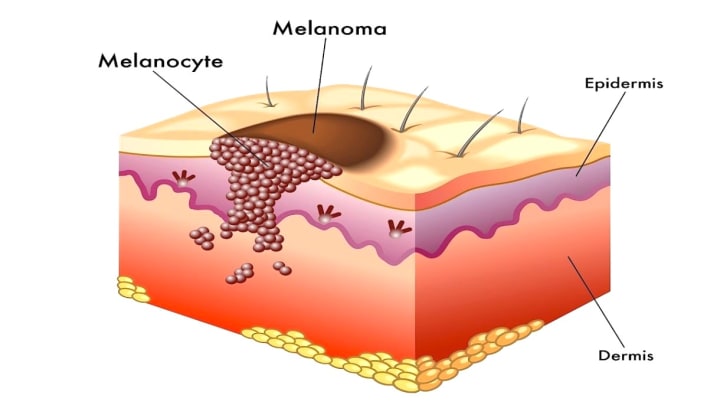
Understanding Melanoma: The Urgency for Innovation
Melanoma makes up just 1% of all skin cancer cases, yet it is blamed for standing behind most skin cancer deaths, as its aggressive ability has an aggressive ability to spread. Unlike basal cell or squamous cell carcinomas, treating melanoma is a real challenge after metastasizing. In Britain, around 16,000 people get to know about melanoma every year, and sadly about 2,300 lost their lives. Even with better treatment, recurrence remains a significant obstacle. However, there is new hope on the horizon! The FDA has recently given the green light to TIL therapy and individual vaccines. These innovative, targeted therapy shows great promise, not only to help patients with melanoma but also to combat other cancers as well as under the line.
How the Trial Works: Precision Meets Accessibility
Eligibility and Recruitment
Potential participants are identified through specialized cancer centers and National Health Service (NHS) cancer clinics. Priority is given to patients with surgically removed Stage III or IV melanoma or those who are at a significant risk of the cancer coming back. The treatment process begins with a genomic examination of the patient's tumor to pinpoint unique neoantigens – essentially, these are mutated proteins that the immune system can identify. This information is then utilized to create personalized cancer vaccines, designed to boost the immune system's response and minimize the chances of relapse in high-priority melanoma patients who are enrolled in cutting-edge treatment trials.
Vaccine Development and Administration
After mapping a patient's tumor profile, a personalized vaccine is created. Rather than using a traditional needle, the ISCIB1+ vaccine is administered through a needle-free jet injection system, which painlessly delivers the vaccine directly into the skin. This innovative approach enhances patient comfort and boosts vaccine absorption, resulting in a more efficient and less aggressive immune response against the cancer, ultimately promoting the body's ability to fight the disease more effectively.
Ongoing Monitoring and Follow-Up
Regularly examined by scans, blood tests, and immune profiles for several months. Close follow-up is to check whether the vaccine has caused a permanent immune response. The ultimate goal is to give time to the immune system to prevent recurrence to identify and eliminate cancer cells with the help of low possibilities of recurrence and repetition to increase long-term existence.
Scientific Credibility: Backed by Research and Institutions
Scancell, a leading biotech firm, has dedicated more than ten years to developing DNA-based immunotherapies. Their innovative iSCIB1+ vaccine is the result of extensive research, which includes promising results from preclinical studies and positive outcomes in Phase I/II clinical trials. The trial demonstrated enhanced survival rates and fewer relapses in cancer patients who received the vaccine, suggesting its potential both as a new tool for cancer prevention and as a long-term treatment through personalized immunotherapy strategies.
The initiative is backed by world-class institutions including:
- Oxford University’s Jenner Institute
- NHS England
- The UK Medicines and Healthcare products Regulatory Agency (MHRA)
- Cancer Research UK
Collectively, these institutions ensure rigorous inspection, scientific reliability, and moral transparency during the testing process.
The Role of the Cancer Vaccine Launch Pad
NHS Cancer Vaccine Launch Pad (CVLP) is an electronic device designed to simplify the recruitment process for cancer vaccine clinical trials across the UK. It only indicates appropriate participants by aligning unknown health records with testing requirements in seconds. It speeds up enrollment, cuts red tape, and shortens the waiting list. Committed to broadening the test access, the platform focuses on attaching to those who often lack representation in such studies. By supporting tests, including people for melanoma, CVLP carried forward medical vaccines that train the immune system to deal with cancer and promote public participation.
Patients' Stories: A New Dawn of Hope
James O’Connor, 58, Leeds
Back in 2022, James was diagnosed with Stage III melanoma. He underwent surgery following immunotherapy. Even though he was later declared cancer-free, the constant fear of the cancer returning loomed over him. He's currently involved in a clinical trial and has shared his experience.
"The idea that my immune system can be trained to fight off cancer is both humbling and empowering. The needle-free injection was quick and painless, and I feel like I’m part of something truly historic."
Layla Hassan, 32, Birmingham
Laila, mom to two fitness instructors, was at first on the fence about joining the trial. However, once she understood the personalized approach of the vaccine, she felt at ease.
"It feels like the future. Instead of a one-size-fits-all drug, this vaccine is designed just for me. I’m grateful for the NHS giving us access to such cutting-edge care without cost."
Expert Opinions: What Medical Leaders Are Saying
Dr. Emily Rhodes, lead oncologist at Manchester Cancer Centre, states:
“We are entering a new era of cancer care. Cancer vaccines, particularly for hard-to-treat cases like melanoma, can complement traditional treatments and provide long-term protection through immune memory.”
Professor Alan Byrne, immunologist and vaccine researcher, adds:
“The precision and safety profile of DNA-based vaccines like iSCIB1+ are immensely promising. The NHS taking a proactive role in rolling this out nationally is unprecedented — and deeply needed.”

A Milestone for Global Healthcare
Individualized cancer vaccines for melanoma have yielded particularly encouraging results, marking a significant success in cancer care. These vaccines work by targeting each patient's unique tumor profile, effectively empowering the immune system to combat the disease. Clinical trials have demonstrated high efficacy and a long-term ability to prevent recurrence. The UK's integration of this approach through the NHS serves as a global example, with countries like Germany, Canada, and Australia closely observing its implementation. This initiative may soon expand to other cancers, including breast, pancreatic, and lung cancer.
Challenges Ahead: Cost, Scalability, and Long-Term Data
Although there's a sense of hopefulness, specialists warn that the broad use of personalized cancer vaccines is still full of challenges:
- Cost and manufacturing logistics: Making thousands of vaccines tailored to individual patients on a large scale demands substantial biotechnological know-how and financial backing.
- Long-term efficacy data: It will be crucial to track clinical results closely to verify that these vaccines provide lasting immune memory and protection over time.
- Public understanding: Clear and straightforward communication about the safety, ethical considerations, and potential advantages of cancer vaccines will be essential to prevent the spread of false information.
Even with these hurdles, the NHS's bold move offers a glimmer of optimism - not just for those battling melanoma, but for cancer patients and researchers worldwide.
Conclusion: A Landmark Step Toward the Future of Cancer Care
The NHS's trial of a skin cancer vaccine signifies more than just a medical breakthrough - it's a major social and scientific milestone. Thanks to cutting-edge research, collaborative partnerships, and a commitment to fair access, the UK is spearheading a shift towards personal, preventative, and patient-centric healthcare. As this program grows, it has the potential to transform countless lives and reshape how we approach cancer treatment. This initiative moves us closer to a future without cancer, establishing a worldwide benchmark for innovative and inclusive healthcare.
About the Creator
UMME HANY
A professional writer is skilled in content creation, SEO writing, & translation. I craft engaging stories on lifestyle, wellness, love, culture & more—blending creativity, clarity, empathy & passion for truly impactful communication.






Comments
There are no comments for this story
Be the first to respond and start the conversation.