When to Worry About Leg Pain
A Simple Guide to Understanding and Preventing DVT
Alex's Story - A Wake-Up Call
Alex, a 42-year-old marketing executive, had always been healthy. He exercised regularly, ate well, and rarely missed work. But everything changed after a business trip to Tokyo. The 14-hour flight left him stiff and sore, but he shrugged it off as normal travel fatigue. Over the next few days, his left calf began to ache - a persistent, deep throb that felt like a muscle strain. By day five, his leg was swollen to twice its size, warm to the touch, and tinged an alarming reddish-purple. When he suddenly struggled to catch his breath while making coffee, his wife insisted on the ER.

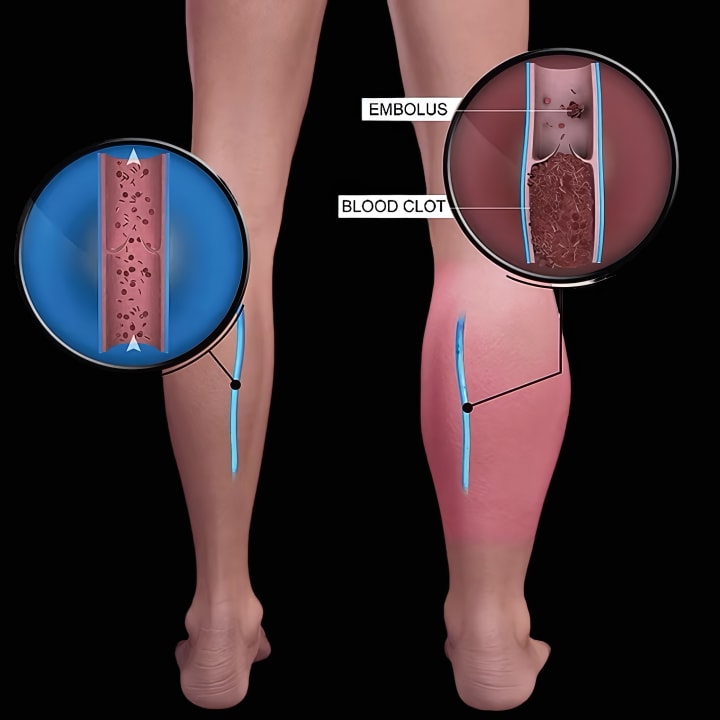
At the hospital, an ultrasound revealed a blood clot in his left calf - deep vein thrombosis (DVT). Worse, a piece of the clot had broken off and traveled to his lung, causing a pulmonary embolism (PE). Alex spent three days in the hospital on blood thinners and oxygen. "I thought I was just tired," he said. "I had no idea my life was in danger."
Alex's story is common but preventable. Let's break down what DVT is, when to worry, and how to protect yourself.
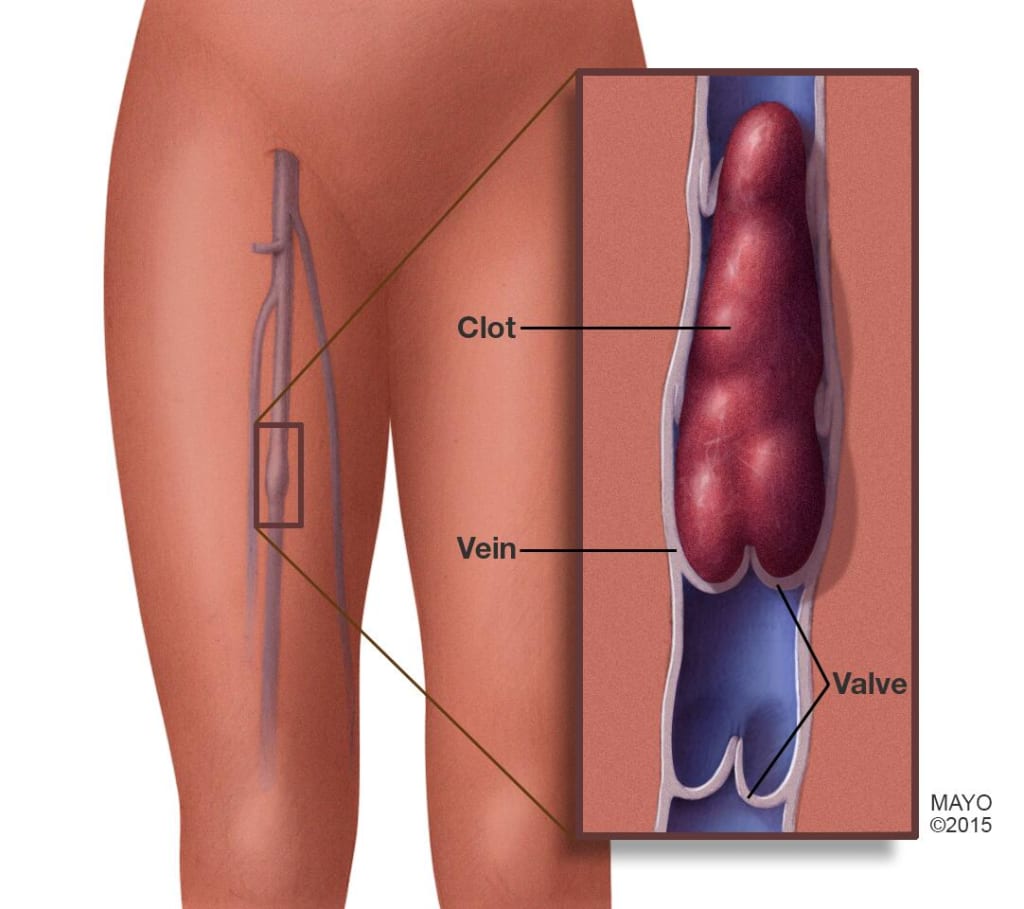
What is DVT?
Deep Vein Thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in the legs. These clots can block blood flow, damage veins, or - in the worst cases - break loose and travel to the lungs (PE) causing life-threatening emergencies.

Why It Matters?
- 500,000+ Americans develop DVT/PE yearly.
- 100,000+ deaths occur annually from PE.
- 50% of DVT cases have no obvious symptoms, making awareness critical.
When to Worry - Recognizing the Signs
DVT symptoms often mimic minor aches, but key differences exist:
Red Flags in Your Leg:
1. Swelling in One Leg
Sudden, unexplained swelling in one calf or thigh (rarely both).
- Example: Sarah, a teacher, noticed her right ankle looked "puffy" after a long drive. She dismissed it until her shoe no longer fit.
2. Pain That Won't Quit
- A cramping or soreness deep in the muscle, often worsening when standing or walking.
- Unlike a muscle strain, DVT pain doesn't improve with rest or stretching.

3. Skin Changes
- Red, purple, or blotchy skin.
- The area may feel warmer than the rest of your body.
4. Veins That Pop Out
- Surface veins might appear more prominent.
Emergency Symptoms (Pulmonary Embolism)
- Sudden shortness of breath (even at rest).
- Chest pain that worsens with deep breaths.
- Coughing up blood or rapid heartbeat.
- Dizziness or fainting.
What to Do Immediately - A Step-by-Step Guide
Step 1: Don't Panic, But Act Fast
- If you have leg symptoms plus breathing issues: Call 911.
- If symptoms are mild but fit DVT patterns: Visit urgent care or your doctor within 24 hours.
Step 2: Prepare for Your Appointment
- Note when symptoms started.
- List recent triggers: flights, surgeries, injuries.
- Share family history of clots.
Step 3: Understand the Tests
- Ultrasound: Painless, 20-minute scan to detect clots.
- D-Dimer Blood Test: Measures clot-dissolving substances (high levels suggest clotting).
- CT Scan or MRI: Used if PE is suspected.
Step 4: Treatment - What to Expect
- Blood Thinners (Anticoagulants): Medications like heparin or rivaroxaban prevent clots from growing.
- Compression Stockings: Reduce swelling and improve blood flow.
- In Severe Cases: Clot-busting drugs (thrombolytics) or surgery.

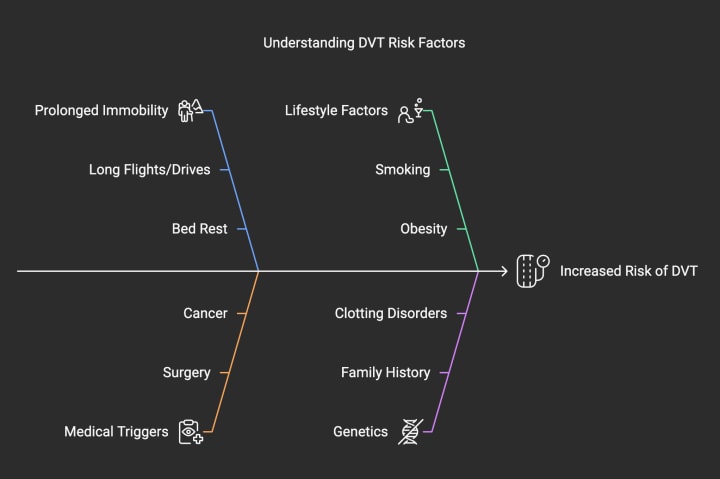
Who's at Risk? - Know Your Vulnerabilities
DVT doesn't discriminate, but these factors raise your risk:
Prolonged Immobility
- Flights/Drives Over 4 Hours: Sitting slows blood flow.
- Bed Rest: After surgery or illness.
Medical Triggers
- Surgery: Especially hip, knee, or cancer surgeries.
- Cancer: Tumors release clot-promoting substances.
- Pregnancy: Hormones + pressure on pelvic veins increase risk.
Lifestyle Factors
- Smoking: Damages blood vessels.
- Obesity: Excess weight strains veins.
Genetics
- Family History: Clotting disorders like Factor V Leiden.
Prevention - Simple Habits That Save Lives
Move Regularly
- On Flights: Stretch hourly; try calf raises or ankle circles.
- At Work: Set a timer to stand/walk every 30 minutes.
Stay Hydrated
- Dehydration thickens blood. Aim for 8 glasses of water daily.
Wear Compression Socks
- Graduated compression (15–20 mmHg) boosts circulation.
Know Your Body
- Post-Surgery: Ask about blood thinners if you're immobile.
- During Pregnancy: Monitor swelling and report pain.
Healthy Lifestyle
- Exercise: Walking, swimming, or yoga improves circulation.
- Quit Smoking: Even vaping harms blood vessels.
Pro Tip: Frequent traveler? Do the "airplane yoga" routine: seated marches, neck rolls, and foot pumps.
Long-Term Management - Life After DVT
Most people recover fully, but some need ongoing care:
- Blood Thinners: May continue for months or years.
- Regular Check-Ups: Monitor for new clots or side effects.
- Mental Health: Anxiety about recurrence is common. Therapy helps.
Myths vs. Facts - Debunking DVT Misconceptions
Myth: "Only older people get blood clots."
Fact: DVT can strike at any age. Instagram influencer Zoe, 24, developed clots after using hormonal birth control.
Myth: "Aspirin can prevent DVT."
Fact: Aspirin isn't enough. Blood thinners are required for treatment.
Myth: "Massaging a swollen leg helps."
Fact: Massage could dislodge a clot! Avoid until cleared by a doctor.
Frequently Asked Questions
Q: Can DVT go away on its own?
A: Small clots might dissolve, but untreated DVT risks PE. Always get checked.
Q: Is flying safe after DVT?
A: Yes, with precautions: compression socks, hydration, and movement.
Q: Can I exercise with DVT?
A: After treatment, yes! Low-impact activities like swimming are ideal.
Final Thoughts: Your Body, Your Lifeline
DVT is stealthy but beatable. Trust your instincts - if something feels wrong, act. Share this guide with frequent travelers, office workers, or loved ones recovering from surgery. As Alex says, "Awareness saved my life. Pass it on."
Remember:
- Swelling + Pain + Warmth = See a doctor.
- Chest Pain + Breathlessness = Call 911.
About the Creator
Mohammad Barbati
Mohammad E. Barbati, MD, FEBVS, is a consultant vascular and endovascular surgeon at University Hospital RWTH Aachen. To date, he has authored several scientific publications and books regarding vascular and venous diseases.






Comments
There are no comments for this story
Be the first to respond and start the conversation.