Thalassemia: Understanding the Silent Blood Disorder
Causes, Symptoms, Prevention, and the Ongoing Battle Against a Hereditary Blood Disease"
Thalassemia: Understanding the Silent Blood Disorder
Causes, Symptoms, Prevention, and the Ongoing Battle Against a Hereditary Blood Disease
Thalassemia, often dubbed a "silent" or "invisible" disorder, is a genetic blood condition that affects the body’s ability to produce hemoglobin—a crucial protein in red blood cells responsible for transporting oxygen throughout the body. Though common in specific parts of the world, thalassemia remains under-recognized and under-researched in many regions, despite its potentially life-threatening implications. With modern medical science making strides in genetics and treatment protocols, it is more important than ever to understand this condition at both a personal and global health level.
---
What is Thalassemia?
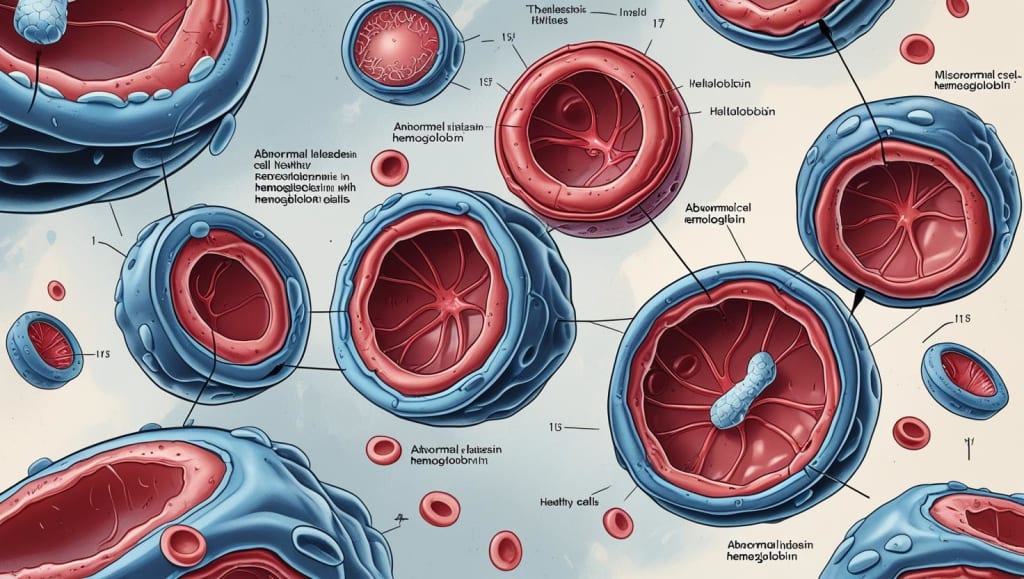
Thalassemia is a group of inherited blood disorders characterized by abnormal or inadequate production of hemoglobin. The disorder primarily affects populations in the Mediterranean, Middle East, Africa, South Asia, and Southeast Asia. It is passed from parents to children through defective genes that affect hemoglobin synthesis.
There are two main types of thalassemia:
Alpha Thalassemia: Caused by mutations in the genes responsible for making alpha-globin chains.
Beta Thalassemia: Resulting from mutations in the beta-globin gene.
Both forms can range from mild (thalassemia minor or trait) to severe (thalassemia major, also known as Cooley’s anemia). Severe cases can lead to life-threatening anemia, organ damage, and other complications.
---
Symptoms and Diagnosis
The symptoms of thalassemia can vary widely depending on the type and severity. Common symptoms include:
Fatigue and weakness
Pale or yellowish skin
Bone deformities, especially in the face
Delayed growth and development
Enlarged spleen
Dark urine
Mild forms may go unnoticed until routine blood tests reveal anemia. More serious cases typically present within the first two years of life.
Diagnosis often involves:
Complete blood count (CBC)
Hemoglobin electrophoresis
Genetic testing to identify specific mutations
Iron studies (to rule out iron-deficiency anemia)
Early diagnosis is crucial, especially in children, as it allows for prompt treatment and prevention of complications.
---
Causes and Genetic Mechanism
Thalassemia is caused by mutations in the DNA of cells that make hemoglobin. These mutations are inherited in an autosomal recessive pattern, meaning a child needs to inherit the defective gene from both parents to develop severe forms of the disease. Carriers (those with one mutated gene) usually have no symptoms or mild anemia but can pass the gene on to their offspring.
Recent genetic research has helped map the mutations responsible for thalassemia more accurately. Scientists have identified over 200 different mutations in the beta-globin gene alone. This genetic diversity explains the variability in symptoms among patients.
---
Treatment and Management
There is no universal cure for thalassemia, but advances in medical science have significantly improved patient outcomes. Treatment depends on the type and severity of the disorder.
1. Regular Blood Transfusions
Used for moderate to severe thalassemia, transfusions help maintain normal hemoglobin levels but can cause iron overload, which must be managed carefully.
2. Iron Chelation Therapy
Patients undergoing frequent transfusions accumulate excess iron, which can damage organs. Drugs like deferoxamine, deferasirox, and deferiprone are used to remove this excess iron.
3. Folic Acid Supplements
Support red blood cell production, especially in patients with mild anemia.
4. Bone Marrow or Stem Cell Transplant
Currently the only potential cure, particularly effective in children. Success depends on having a compatible donor, usually a sibling. New research is exploring the use of haploidentical transplants (partially matched donors) with encouraging results.
---
Advanced Research and Emerging Therapies
In recent years, scientific advances have opened new frontiers in the treatment of thalassemia:
1. Gene Therapy
One of the most exciting developments. In 2022, the FDA approved a gene therapy called Zynteglo (betibeglogene autotemcel) for patients with beta-thalassemia who require regular transfusions. This therapy involves inserting a functional beta-globin gene into the patient’s stem cells, which then begin producing healthy red blood cells. Clinical trials have shown that many patients were able to stop transfusions entirely.
2. CRISPR and Genome Editing
CRISPR-Cas9 technology is being tested to correct the genetic defects at their source. Trials like CTX001, a CRISPR-based therapy developed by Vertex and CRISPR Therapeutics, have shown promise in reducing or eliminating transfusion dependence.
3. Pharmacological Agents
New drugs are being developed to increase fetal hemoglobin (HbF) levels, which can compensate for the defective adult hemoglobin. Luspatercept, approved by the FDA, helps reduce the frequency of transfusions in adults with beta-thalassemia by improving red blood cell maturation.
---
Prevention Through Genetic Counseling
Given that thalassemia is inherited, prevention strategies rely heavily on education and screening:
Carrier Screening Programs: Especially in high-risk regions or communities, to identify potential carriers before marriage.
Prenatal Testing: Chorionic villus sampling and amniocentesis can detect thalassemia in fetuses.
Preimplantation Genetic Diagnosis (PGD): For couples undergoing IVF, PGD can help select embryos without the thalassemia gene.
Countries like Cyprus, Iran, and Italy have implemented national prevention programs, significantly reducing the number of new thalassemia major births.
---
Living with Thalassemia
Thanks to improved care, many individuals with thalassemia now live well into adulthood. However, long-term challenges remain:
Maintaining treatment adherence
Managing psychological and social impacts
Dealing with the cost of care
Support groups, patient advocacy organizations, and access to comprehensive care are vital to improving quality of life.
---
Conclusion
Thalassemia, while complex and often lifelong, is no longer a mysterious or untreatable condition. With cutting-edge therapies like gene editing, the future is brighter than ever for those affected. However, awareness, early diagnosis, and prevention through genetic counseling remain key tools in reducing its global burden. As research progresses, the hope for a universal cure becomes increasingly tangible—turning what was once a silent killer into a manageable, and potentially curable, disease.
About the Creator
Hasbanullah
I write to awaken hearts, honor untold stories, and give voice to silence. From truth to fiction, every word I share is a step toward deeper connection. Welcome to my world of meaningful storytelling.





Comments
There are no comments for this story
Be the first to respond and start the conversation.