Making Thanksgiving Inclusive for Loved Ones With Communication and Swallowing Challenges
Supporting Family and Friends With Parkinson’s, Stroke Recovery, Aphasia, Dysphagia, Traumatic Brain Injury, and Progressive Neurological Conditions

Thanksgiving brings families together.
But for those with neurological conditions like stroke, Parkinson's disease, aphasia, dysphagia, or traumatic brain injury, the holiday can bring unique challenges alongside its joys.
Whether this is your first Thanksgiving since a loved one's diagnosis or you're navigating progressive changes, a few thoughtful accommodations can transform the experience for everyone.
This article distills key insights on accommodating family and friends with speech-therapy-related deficits at Thanksgiving, focusing on practical strategies you can implement immediately to support loved ones with communication, swallowing, and cognitive challenges.
Create a Supportive (Not Overwhelming) Environment
The physical environment profoundly impacts someone's ability to engage comfortably at Thanksgiving.
Many neurological conditions affect sensory processing, making the typical holiday chaos: overlapping conversations, background music, flickering candles, and constant movement are all genuinely overwhelming rather than festive.
What feels like warm ambiance to you might trigger sensory overload, fatigue, or anxiety for someone managing communication or cognitive challenges.
The solution isn't sterile silence, but rather thoughtful environmental design. Reducing background noise allows people with dysarthria (unclear speech from conditions like Parkinson's) to be heard and understood.
Consistent lighting helps those with visual processing difficulties navigate safely. Predictability, things like knowing when dinner will be served, who's coming, where they'll sit, reduces the cognitive load for people with memory challenges or TBI-related executive function difficulties.
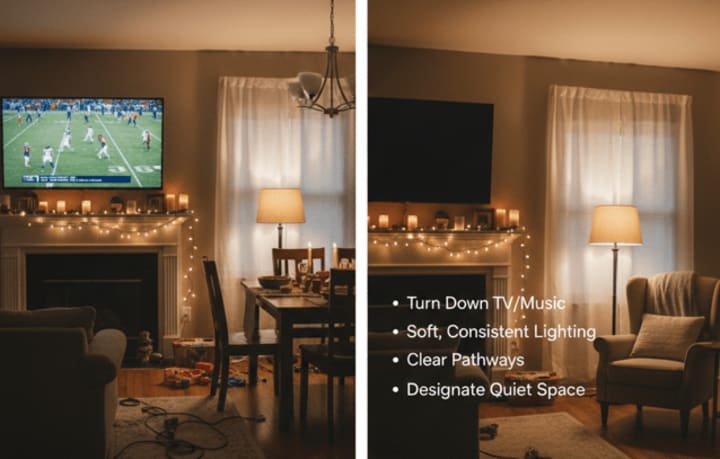
Consider these foundational adjustments:
Reduce sensory overwhelm:
- Turn down background TV and music during conversations
- Provide soft, consistent lighting without flickering candles
- Designate a quiet room where anyone can retreat to rest
Ensure safety and comfort:
- Clear pathways of clutter for those with mobility challenges
- Share the day's schedule in advance to reduce anxiety
- Keep seating areas calm and spacious
These small adjustments make a dramatic difference for people with sensory processing difficulties or fatigue.
Support Communication With Patience and Respect

Perhaps the most isolating aspect of neurological conditions isn't the physical challenges. Rather, it's feeling disconnected even in a room full of family.
Communication difficulties don't reflect intelligence or comprehension; they reflect neurological changes that disrupt language access, speech production, or information processing.
- Someone with aphasia from a stroke knows exactly what they want to say but can't access the words.
- Someone with Parkinson's dysarthria has clear thoughts but can't produce clear speech.
- Someone with TBI-related cognitive changes may struggle to organize their thoughts or follow rapid conversational turns.
The key to supporting communication is understanding that different conditions require different strategies, while some universal principles help everyone. Speaking naturally, not loudly or in exaggerated child-directed speech, preserves dignity while remaining clear.
Giving time for responses honors the reality that processing and formulating language takes longer after neurological injury. Confirming understanding without making it feel like a test ("Did you say you'd like coffee?") ensures accurate communication while maintaining respect.
Universal principles that help everyone:
- Speak naturally, not loudly or slowly like you're talking to a child
- Give time for responses: silence is processing time, not a cue to interrupt
- Ask simple yes/no questions when appropriate
- Confirm what you heard without making it feel like a test
For people with aphasia (difficulty finding or understanding words):
- Offer choices: "Coffee or tea?" instead of "What would you like?"
- Use gestures, written words, or photos to support communication
- Never finish their sentences unless they ask you to
For people with soft or unclear speech:
- Position yourself face-to-face to hear better
- Reduce background noise when they're speaking
- Repeat back what you understood to confirm
For people with memory challenges:
- Introduce yourself warmly: "Hi, I'm Nina, Giovanni's daughter!"
- Provide context naturally without correcting: "We're at my house for Thanksgiving"
- Keep conversations in small groups of 2-3 people
What never to say:
- "You sound so different"
- "Do you remember me?"
- "Just try harder to talk"
- "You're not eating much"
Make Dining Comfortable and Safe for All

Thanksgiving dinner often becomes the most stressful part of the day for people with neurological conditions, and it's not because of the menu.
Eating in front of others feels vulnerable when you have tremor that makes utensils shake, dysphagia that requires careful swallowing, or cognitive changes that make using silverware confusing.
Simple adaptive equipment preserves independence, which also preserves dignity. Weighted utensils compensate for tremor without calling attention to it. Non-slip placemats stabilize plates so food doesn't slide away. High-sided bowls make scooping easier for those with motor challenges.
For those with dysphagia (swallowing difficulties), safety must be balanced with dignity and enjoyment. This doesn't mean bland puréed everything served in obviously "special" bowls. It means understanding which traditional Thanksgiving foods are naturally dysphagia-friendly:
- Mashed potatoes
- Stuffing with gravy
- Well-cooked sweet potatoes
- Pumpkin pie
It also means pre-cutting foods to appropriate sizes in the kitchen, not at the table. It means providing adequate moisture through gravies and sauces rather than dry textures that increase choking risk.
Strategic seating matters:
- Seat loved ones at the end of the table to reduce overwhelm
- Place them near patient, understanding family members
- Keep them away from high-traffic kitchen areas
Support independence discreetly:
- Provide weighted utensils for tremor or built-up handles for weak grip
- Use non-slip placemats and high-sided bowls
- Offer to plate food in the kitchen to avoid the pressure of a busy table
For those with swallowing difficulties (dysphagia):
- Ensure they're seated fully upright
- Pre-cut foods into small, manageable pieces
- Provide moist textures: gravies, sauces, well-cooked vegetables
- Never comment on eating pace or pressure them to "just try a bite"
- Understand that some coughing may be normal, so stay calm unless it escalates
Serve modifications subtly:
- Don't announce "special dietary needs" to the table
- Use regular dishes, not obviously separate plates
- Offer naturally soft foods like mashed potatoes, stuffing, and pumpkin pie alongside traditional options
Include Everyone in Activities Away from the Table

Thoughtful activity planning creates opportunities for genuine connection without pressure. Conversation works better in small groups of two to three people rather than large table discussions where turn-taking happens rapidly.
Memory-based questions ("What was Thanksgiving like when you were growing up?") often work better than current-event topics because long-term memories typically remain more accessible. Visual prompts, like photo albums, objects, or the football game on TV, anchor conversations and reduce language demands.
TIP: Activities associated with PACE Therapy often translate well into communicative activities with family, not just aphasia patients.
Activities should allow flexible participation, meaning people can engage deeply or peripherally based on their energy and comfort. Watching football together provides shared experience without demanding constant conversation.
Looking through photo albums supports communication through visual prompts. Simple crafts like folding napkins or arranging flowers provide purposeful activity without complex verbal instructions.
Conversation topics that work well:
- Memory-based questions: "What was Thanksgiving like when you were growing up?"
- Photo albums or pictures on your phone
- Watching football or the parade together
Low-pressure activities:
- Looking through family photos
- Simple tasks like folding napkins or arranging flowers
- Watching games or shows together without requiring constant conversation
- Gentle movement like a short walk if weather permits
Respect energy levels:
- Normalize rest breaks without calling attention to them
- Don't hover or repeatedly ask "Are you okay?"
- Let people participate at their own pace and leave when comfortable
Don't Forget the Caregiver: It's Their Holiday Too!

Behind every person with a neurological condition is often a caregiver who's exhausted, stressed, and still putting on a smile for the holidays.
Caregivers typically haven't had a break in months, feel responsible for everything going smoothly, and often neglect their own needs while managing complex care demands.
At Thanksgiving, they're often hyper-vigilant about their loved one's safety, comfort, and social experience, which means they rarely relax enough to enjoy the gathering themselves.
The most helpful thing you can do is offer specific, concrete support rather than vague "let me know if you need anything" statements that rarely get taken up.
Offering to sit next to their loved one during dinner gives the caregiver permission to eat without constant vigilance. Volunteering to prepare the dysphagia-safe plate removes one decision-making burden. Taking over mobility assistance for bathroom trips provides a genuine break.
Offer specific help:
- "I'd love to sit next to your mom during dinner so you can eat worry-free"
- "Can I prepare her plate?"
- "Why don't you take a break? I'll keep him company"
- "What can I do to make today easier for you?"
Vague offers like "let me know if you need anything" rarely get taken up. Be specific and proactive.
The Bottom Line: Dignity First This Thanksgiving

Every accommodation should serve one purpose: supporting your loved one without spotlighting their challenges.
The goal is connection. When you lead with patience, empathy, and respect, you create a Thanksgiving where everyone feels they belong exactly as they are.
Your loved one may communicate differently now. They may need different foods or more time. But their fundamental place in your family hasn't changed. This Thanksgiving, affirm that they belong at your table and in your heart.
The accommodations we've discussed aren't about treating someone as fragile or broken. They're about removing barriers so the person you love can fully participate in family traditions. They're about making space for different abilities while maintaining the warmth and meaning that make Thanksgiving special.
You now have an extensive guide to accommodating family and friends with speech-therapy-related deficits at Thanksgiving that addresses Parkinson's, stroke recovery, aphasia, dysphagia, TBI, dementia, and progressive neurological conditions in comprehensive detail.
Whether this is your first Thanksgiving navigating these challenges or you're refining approaches you've developed over years, the most important thing you bring to the table is love, patience, and the commitment to genuine inclusion.
This article is intended for informational purposes. Always consult with healthcare providers and speech-language pathologists for individualized recommendations.
About the Creator
Nina Minervini
I write about the real-world side of speech therapy: the challenges, the breakthroughs, and the moments that remind us why communication matters. My stories highlight the progress and the practical ways SLPs help families every day.






Comments
There are no comments for this story
Be the first to respond and start the conversation.