What is the relationship between trauma and mental health disorders?
relationship between trauma and mental health

Trauma is any profoundly disturbing or upsetting experience that overwhelms an individual's capacity to cope, leaving a permanent emotional, psychological, and frequently physical health imprint. Trauma can result from one isolated event—a car accident, tornado, or assault—or from long-term exposure to adversity, such as child abuse, domestic violence, or life in a combat zone.
Though not everyone who experiences trauma will end up with a mental illness, there is a robust and proven relationship between trauma and the occurrence of psychological disorders, including post-traumatic stress disorder (PTSD), depression, anxiety, substance use disorders, and dissociative disorders. Awareness of this association is essential in promoting healing, building resilience, and providing proper treatment for individuals affected.
Understanding Trauma
Trauma impacts the threat response system of the brain, including the amygdala, hippocampus, and prefrontal cortex—the regions that deal with emotion regulation, memory, and decision-making. As an individual undergoes trauma, the brain is capable of being "stuck" in hyperarousal state, reenacting memories, sensations, or fear long after the incident has passed.
Trauma can be categorized into several subtypes:
Acute trauma: triggered by one-time incident (e.g., assault, accident)
Chronic trauma: the result of repeated and extensive exposure to distress (e.g., abuse, domestic violence)
Complex trauma: repeated exposure to multiple traumatic events, often intrusive and interpersonal (e.g., childhood neglect, trafficking)
Importantly, trauma is self-defined—what is traumatic to one person may not be to another. It's the person's internal response, and not the event itself, that defines the impact.
Mental Health Disorders Linked to Trauma
1. Post-Traumatic Stress Disorder (PTSD)
PTSD is probably the most well-known trauma-related psychiatric disorder. PTSD occurs if an individual continues to experience severe psychological distress after a traumatic event has occurred. Symptoms may involve:
Intrusive flashbacks or recollections
Nightmares
Avoidance of reminders or cues
Exaggerated startle and hypervigilance
Emotional numbness or detachment
Negative worldview or self-perceptions
PTSD does not only impact military veterans or first responders—survivors of accidents, abuse, violence, or even witnessing become involved.
2. Complex PTSD (C-PTSD)
C-PTSD is usually the result of chronic and prolonged trauma, especially if this occurs during childhood. In addition to PTSD symptoms, the individual may have:
Long-standing shame, worthlessness, or guilt feelings
Difficulty with emotion regulation
Troubles with others or in relationships, such as fear
Dissociation or loss of memory
It is often misdiagnosed or underdiagnosed, especially in groups with chronic histories of childhood neglect or abuse.
3. Depression
Trauma acutely increases the risk for developing major depressive disorder. The emotional load of trauma can lead to:
Hopelessness and sadness
Loss of interest or pleasure
Fatigue and withdrawal
Suicidal ideation or self-injury
Research confirms that childhood trauma is a strong risk factor for depression in adulthood in the long term.
4. Anxiety Disorders
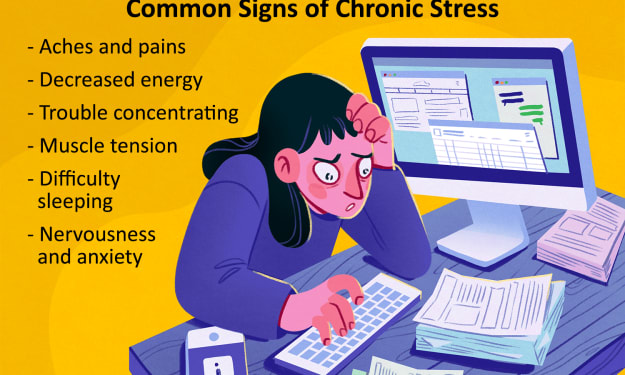
Trauma can disrupt the nervous system's ability to relax, causing chronic frightfulness or panic disorders. The individual can experience:
Excessive fearfulness or anxiety
Difficulty relaxing
Sleep disturbances
Physical complaints such as nausea or chest pain
Even years later, subtle cues trigger massive frightfulness.
5. Dissociative Disorders
In order to cope with severe trauma, especially during childhood, the mind can "dissociate," or disconnect from reality. Symptoms of dissociative identity disorder (DID) or dissociative amnesia may include:
Memory gaps or blackouts
Being detached from one's body (depersonalization)
Being detached from the world around oneself (derealization)
Feeling a different sense of identity
Dissociation is adaptive, but it can impair emotional processing and relationships in the long run.
6. Substance Use Disorders
Many survivors of trauma use alcohol, drugs, or prescription medication to numb emotional suffering. Although they may initially bring comfort, they often lead to addiction and worsen mental illness.
Why Trauma Affects People Differently
Few people who have experienced trauma go on to develop a mental illness. The following factors influence how an individual responds:
Genetics and heredity of mental illness
Age the trauma occurred (early trauma has more long-lasting effect)
Access to emotional support and support system
Coping skills and resilience skills
Character of the trauma (repeated or single, intentional or unintentional)
Presence of protective factors, such as therapeutic support, safe environment, and caring caregiver, can buffer against lasting harm.
The Importance of Trauma-Informed Care
Comprehending the role of trauma is central to effective mental health care. Trauma-informed care is a system that embraces the endemic nature of trauma and brings this information to bear on every aspect of patient care. Its values are:
Safety: Creating an environment in which clients feel physically and emotionally safe
Trustworthiness and transparency
Peer support
Collaboration and empowerment
Cultural, historical, and gender sensitivity
This strategy rephrases the question from one of judgment and shame .
Healing from Trauma: Treatment and Recovery
While the effects of trauma might be long-lasting and even transformative, healing is always an option. Recovery often entails some combination of professional therapy, personal growth, and nurturing relationships.
1. Psychotherapy
The following therapies are specifically designed to address trauma:
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): Helps in recognizing and changing negative belief patterns
Eye Movement Desensitization and Reprocessing (EMDR): Involves deliberate eye movement to help in reprocessing traumatic memories
Somatic Experiencing: Focuses on body sensations and awareness to release stored trauma
Internal Family Systems (IFS): Helps in identifying and healing parts of oneself that were affected by trauma
Therapy is a secure environment in which one can confront the pain, develop compassion for oneself, and reauthor the narrative of the trauma.
2. Medication
In some instances, antidepressants or anti-anxiety medication may be given to manage symptoms like panic, intrusive thinking patterns, or severe depression. Medication is most effective when used alongside therapy.
3. Self-Care and Grounding
Recovery from trauma is not just a process of verbalization but also reconnecting with the body, implementing safety, and re-establishing a sense of agency. Grounding techniques involve:
Deep breathing or meditation
Journaling
Art therapy
Moving practices like yoga or tai chi
Spending time outdoors in nature
Having consistent routines and sleep hygiene
4. Support Networks
Talking to trusted friends, joining trauma recovery groups, or consulting with a trauma-informed coach can reduce loneliness. Feeling heard, seen, and believed is a big part of healing—this can make individuals feel safe once more.
Barriers to Healing
Unfortunately, there are numerous barriers to help-seeking for trauma survivors:
Stigma or shame regarding discussion of trauma
Restricted access to mental healthcare
Misunderstanding or misdiagnosis by physicians
Avoidance of painful emotions or memories
Breaking through these barriers of awareness, education, and culturally grounded care is the pathway to systemic change.
Trauma and Hope
Trauma does not define who they are—it's something that has occurred to them, not what they are. Survivors are not broken; they are people who went through something that hurt them and they survived. With good care, healing can transition from surviving to thriving, recovering joy, trust, and connection.
Healing isn't linear and is slow. There can be setbacks, but each step forward in terms of understanding and compassion is a step towards completion. You are not by yourselves, and it is never too late to heal.
For a kinder mental health care and trauma-informed care, consider:
https://www.delhimindclinic.com/
https://www.craftcmsdeveloper.in/
Don't wait to reach out if you need to make changes to your Craft website or just talk about your Craft project. I'd be pleased to provide a free consultation!




Comments
There are no comments for this story
Be the first to respond and start the conversation.