What is Obsessive-Compulsive Disorder (OCD) and how can it be treated?
OCD
Obsessive-Compulsive Disorder, popularly known as OCD, is a long-term mental health disorder that strikes individuals of all ages and backgrounds. Although the label "OCD" is frequently misunderstood or trivialized in everyday speech—like when an individual states that they're "so OCD" because they prefer their workspace tidy—the actual experience of living with OCD is considerably more severe and debilitating. This condition has a cycle of obsessions (involuntary, intrusive thoughts) and compulsions (repetitive behaviors or mental acts that are performed to reduce anxiety).
OCD can significantly interfere with daily functioning, relationships, employment, and overall quality of life. Fortunately, through accurate diagnosis, evidence-based treatments, and supportive care, individuals with OCD can manage their symptoms and enjoy productive lives.
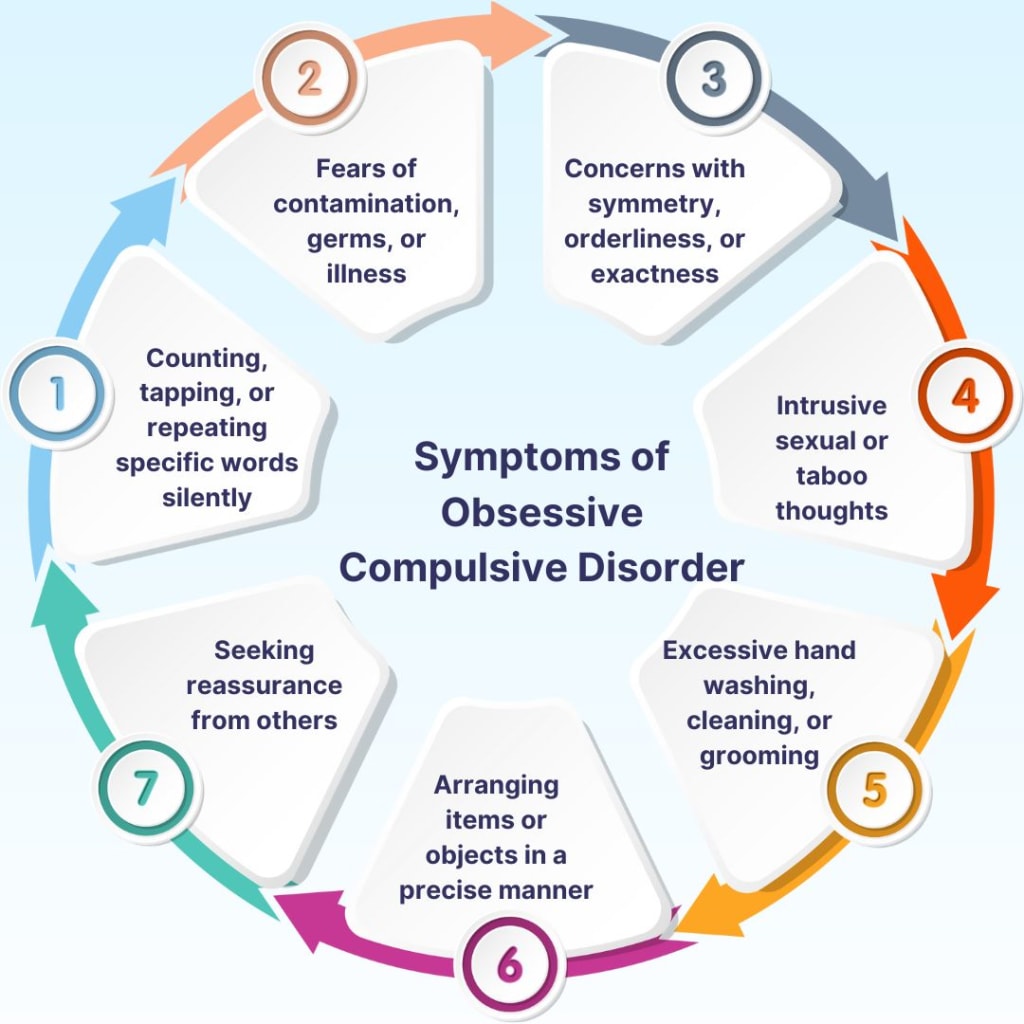
The Symptoms: Obsessions and Compulsions
OCD consists of two primary elements:
1. Obsessions
These are intrusive and persistent thoughts, images, or compulsions that cause significant distress or anxiety. Classic examples are:
Fear of contamination (e.g., germs, dirt, body fluids)
Fear of harming oneself or others
Intrusive thoughts about forbidden topics (e.g., violence, sex, religion)
Need for symmetry, order, or perfection
Excessive doubt and need for reassurance
Obsessions are not worry about real problems in a person's life; they are often irrational and unwanted, and the person experiencing them usually realizes that these thoughts are illogical or excessive.
2. Compulsions
Repeating rituals or mental processes that an individual feels obliged to perform as a response to an obsession. The purpose is typically to reduce anxiety or prevent an awful event or situation from occurring. Some compulsions include:
Excessive hand washing or cleaning
Checking the doors, locks, stoves repeatedly
Repeating words, phrases, activities repeatedly to oneself
Counting, tapping, or lining objects up repeatedly until it "feels right"
Repeatedly seeking reassurance from others
While these behaviors bring temporary relief from distress, they never eliminate the underlying preoccupation and actually reinforce the cycle of OCD.
How OCD Affects Daily Life
The scope of OCD can be extensive. People spend anywhere from one to several hours a day performing compulsions, which results in:
Missed work or school
Distorted relationships from excessive need for reassurance or rituals
Emotional exhaustion from long-term mental distress
Social withdrawal from embarrassment or judgment avoidance
Loss of self-esteem due to emotional feelings of being out of control
In more serious cases, OCD can be disabling, preventing the individual from being able to take care of oneself. Significantly, most people with OCD are aware that their thoughts and behaviors are irrational, something that only contributes to increased feelings of shame and frustration.
What Causes OCD
OCD is a multi-factorial disorder with a combination of biological, psychological, and environmental determinants:
Genetics: OCD is more common in families, suggesting there is a genetic component.
Brain structure and function: Brain imaging research demonstrates abnormalities in the frontal cortex and subcortical areas that are involved in decision making and behavioral control.
Neurotransmitters: Dysfunction in serotonin, a neurotransmitter involved in mood regulation, is thought to play a part.
Life experiences and trauma: Stress, trauma, or major life changes at the childhood stage can trigger or worsen OCD.
Personality styles: Individuals with perfectionism or a high need for control may be more susceptible to developing OCD.
It should be kept in mind that OCD is not caused by bad parenting, weakness, or lack of will power.
Types of OCD
OCD can manifest in multiple forms. Some of the most common subtypes include:
Contamination OCD: Dread of disease or germs, leading to compulsions to clean
Checking OCD: Repeated checking of things like locks, appliances, or email
Symmetry and Order OCD: Things must be arranged or put "perfectly" in position
Harm OCD: Risk of unintentionally or on purpose harming others
Sexual or Religious OCD: Intrusive thoughts about forbidden subjects, with guilt or sinning fear
Pure O (Primarily Obsessional OCD): Individuals experience obsessions with no observable compulsions, typically carrying out mental rituals
Each type of OCD may exhibit differently, but the same obsession → anxiety → compulsion cycle underlies them.
Diagnosis and Misconceptions
OCD is often underdiagnosed or misdiagnosed, at least in part because individuals are too embarrassed to disclose their intrusive thoughts. Some individuals may not even be aware that their mental rituals are actually compulsions. OCD may also become confused with:
Generalized Anxiety Disorder (GAD)
Depression
Phobias
Body Dysmorphic Disorder
Autism Spectrum Disorder (when routines and rituals exist)
A trained mental health clinician can offer a thorough assessment, most commonly with the assistance of structured interviews and standard scales like the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), in an attempt to make the diagnosis.
Effective Treatments for OCD
There is no cure available for OCD, but it can be treated thoroughly through the proper mix of therapy, drugs, and support.
1. Cognitive Behavioral Therapy (CBT)
The most effective therapy for OCD is a form of CBT called Exposure and Response Prevention (ERP). This involves:
Exposure: Gradual exposure to dreaded thoughts, pictures, or situations
Response prevention: Refraining from the urge to perform acts
For example, a person with contamination OCD will touch a doorknob and then struggle to wash hands. Later, this process will teach the mind that the expected result does not occur and the anxiety is reduced.
ERP is challenging but can be very effective if performed constantly with a trained therapist.
2. Medication
Selective Serotonin Reuptake Inhibitors (SSRIs) such as fluoxetine (Prozac), sertraline (Zoloft), or fluvoxamine are frequently employed. These medications regulate serotonin levels and reduce the intensity of obsessions and compulsions.
Higher doses may occasionally be required for OCD than depression, and effects may not be noticed for 8–12 weeks. In treatment-resistant cases, antipsychotic medication or more novel approaches like ketamine may be attempted under medical supervision.
3. Mindfulness and Acceptance-Based Strategies
Mindfulness is also helping individuals observe intrusive thoughts without reaction or judgment, weakening their power over time. Acceptance and Commitment Therapy (ACT) skills are also being utilized to help individuals accept distress without resorting to compulsions.
4. Support Groups and Peer Networks
Being part of an OCD support group can reduce isolation, affirm experience, and supply coping skills. Hanging out with other individuals who "get it" may be absolutely therapeutic.
Self-Care and Lifestyle Support
Treating OCD is not just a matter of medication or therapy; daily habits matter too:
Sleep: Have quality, regular sleep
Nutrition: Eat a healthy diet to support brain health
Exercise: Regular exercise reduces anxiety
Routine: Have a routine to reduce decision fatigue
Stress Management: Create healthy coping mechanisms (drawing, journaling, nature, etc.)
Avoiding alcohol and caffeine, especially when under treatment, can also reduce symptoms.
Supporting a Loved One with OCD
If a loved one suffers from OCD:
Be patient and nonjudgmental
Avoid enabling compulsions (e.g., providing constant reassurance)
Encourage them to seek professional help
Educate yourself about OCD to better understand what they’re going through
Celebrate small wins in their recovery journey
It’s important to support without participating in the disorder’s cycle.
Living with OCD: A Message of Hope
OCD is an ongoing illness, but not a death sentence. With proper treatment and support, most people with OCD can overcome their symptoms, reduce their distress, and reclaim their lives. It is gradual improvement and the setbacks will occur, but each step forward is important.
The courage it takes to confront what scares you, to defeat compulsion, and to speak openly about unwanted thoughts is enormous. Everyone who has OCD is worthy of respect, compassion, and access to high-quality care.
If you or your loved one is experiencing symptoms of OCD, don't hesitate to seek professional assistance. You are not alone—and help is available.
Visit:
https://www.delhimindclinic.com/
https://www.craftcmsdeveloper.in/
Feel free to get in touch with me if you would like to make changes to your Craft site or simply discuss your Craft project. I provide a free consultation!




Comments
There are no comments for this story
Be the first to respond and start the conversation.