Scientists Achieved Breakthrough in Diabetes Cure with Gene-Edited Transplant
Breakthrough Procedure Frees Patient from Insulin Injections and Immune Suppression

Introduction
A remarkable medical achievement has given new hope to people living with type 1 diabetes. Scientists from Sweden and the United States have successfully transplanted genetically modified pancreatic cells into a patient, enabling him to produce insulin naturally without relying on daily injections or powerful drugs. This success, published in the New England Journal of Medicine, could transform the way diabetes is treated in the future.
Understanding Type 1 Diabetes
Type 1 diabetes is an autoimmune disease that affects around 8.4 million people worldwide. In this condition, the body’s immune system mistakenly destroys the insulin-producing beta cells in the pancreas. Since insulin is essential for controlling blood sugar, patients must depend on regular insulin injections or pumps for survival.
While traditional islet cell transplants have shown promise, they come with a major problem: the patient’s immune system usually rejects the transplanted cells. To prevent this, patients need lifelong immunosuppressive drugs. Unfortunately, these drugs weaken the immune system, increasing the risk of infections and other health complications. This makes the treatment unsuitable for large-scale use.
The Innovation: Gene-Edited Cells
To overcome this challenge, scientists turned to advanced gene-editing tools. Using CRISPR-Cas12b, a newer and more precise version of CRISPR technology, they made three key genetic modifications to donor pancreatic cells:
- Hiding from the immune system, they removed two genes that normally produce “antigens,” which alert the immune system to attack.
- Adding a protective shield, they boosted the expression of a protein called CD47, which sends a “don’t attack me” signal to the immune system.
- These changes created what researchers call “immune-evasive” islet cells. In simple terms, these cells can survive inside the body without being destroyed, and without the need for heavy-duty drugs.
The Transplant Procedure
Unlike traditional methods where cells are transplanted into the liver, the research team injected the modified cells into the patient’s forearm muscle. This location was chosen because it is safer and easier to monitor.
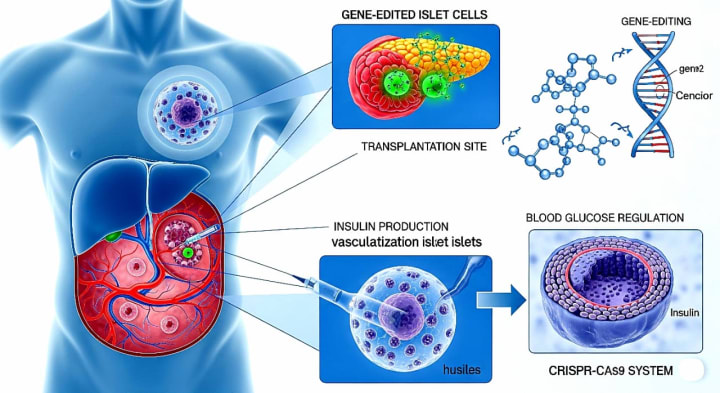
The results were astonishing. Within 12 weeks, the transplanted cells started producing insulin whenever the patient’s blood sugar levels rose. For the first time in years, his body could naturally regulate blood sugar something most people with type 1 diabetes cannot do. Importantly, there were no signs of immune rejection during this period, proving that the gene edits worked as intended.
Why This Matters
This single case may seem small, but it represents a huge step forward. For decades, diabetes treatments have focused on managing symptoms rather than providing a cure. If immune-evasive cell transplants can be perfected, patients may no longer need daily insulin injections or risky immunosuppressive drugs.
Beyond diabetes, this success highlights the power of gene-editing technology in medicine. CRISPR-Cas12b could also be applied to other diseases where the immune system interferes with treatments, opening doors to new forms of regenerative medicine.
The Road Ahead
Despite this exciting progress, researchers stress that the journey is just beginning. This was only a single-patient trial, and much more testing is needed to ensure long-term safety and effectiveness. Future studies will need to answer important questions:
Will the transplanted cells continue to function for years, not just weeks?
Could there be hidden side effects over time?
Can these cells be produced at a scale large enough to help millions worldwide?
How can we ensure fair and affordable access to this advanced therapy?
The success of this gene-edited islet cell transplant is a shining example of what modern science can achieve when different fields gene editing, immunology, and cell therapy come together. While challenges remain, this breakthrough has the potential to free people with type 1 diabetes from the lifelong burden of insulin injections. It is not yet a cure for everyone, but it is a hopeful step toward a future where diabetes may no longer control lives.
About the Creator
Muzamil khan
🔬✨ I simplify science & tech, turning complex ideas into engaging reads. 📚 Sometimes, I weave short stories that spark curiosity & imagination. 🚀💡 Facts meet creativity here!






Comments
There are no comments for this story
Be the first to respond and start the conversation.