Revenue cycle management | Leukocytosis ICD 10
Accurate ICD-10 coding is essential for proper billing, claim processing, and ultimately, getting paid for services rendered.
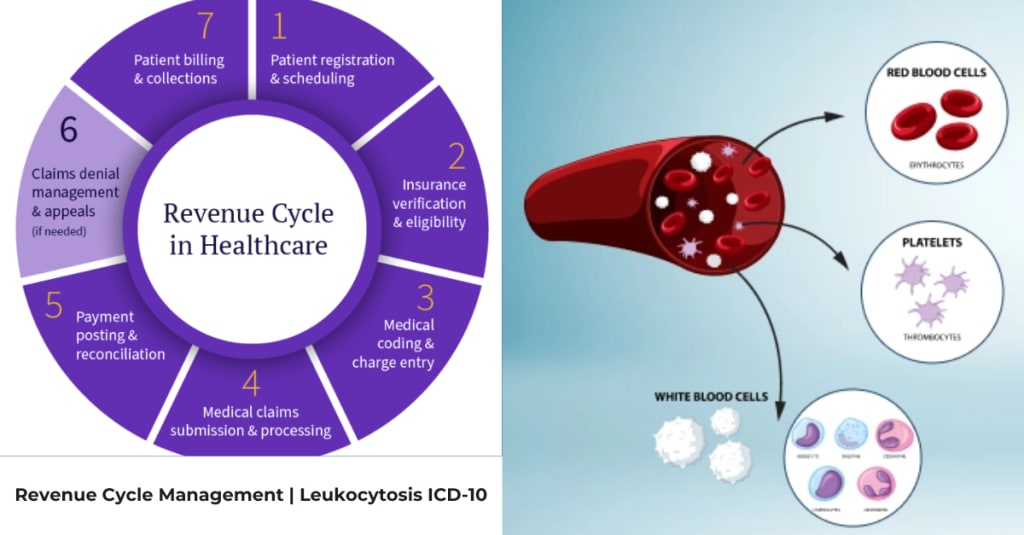
Revenue cycle management (RCM) is the financial process healthcare organizations use to track patient accounts from registration and service delivery to final payment. Its purpose is to maximize reimbursement, streamline administrative tasks, improve efficiency, ensure regulatory compliance, and enhance the patient experience. Key steps include patient scheduling and registration, insurance verification, charge capture, Medical Coding, claims submission, payment processing, and collections.
Core functions of revenue cycle management
- Patient registration and insurance verification: Gathering patient information and confirming insurance eligibility and benefits at the time of service.
- Charge capture and medical coding: Accurately documenting and coding all services provided during a patient's visit to ensure correct billing.
- Claims submission and management: Submitting clean claims to payers (insurance companies and government programs) and following up on denied claims.
- Payment processing: Processing payments from both insurance companies and patients and posting them to the correct accounts.
- Patient billing and collections: Sending clear bills to patients for any remaining balance and managing the collection of those payments.
Benefits of effective RCM
- Improved cash flow: Ensures a stable and reliable income stream for the organization.
- Increased revenue capture: Maximizes reimbursement by minimizing errors and denials.
- Enhanced efficiency: Streamlines administrative workflows, reducing manual work and staff burden.
- Better compliance: Helps the organization stay compliant with complex and changing healthcare regulations.
- Improved patient experience: Creates a more transparent and straightforward billing process for patients.
Medical Billing and Coding:
Medical billing is the comprehensive process healthcare providers use to submit and follow up on claims with health insurance companies and patients to receive payment for services rendered. It is a critical part of the healthcare industry's revenue cycle, ensuring financial stability for providers while facilitating patient access to care.
The Medical Billing Process
The medical billing process, often called the billing cycle, involves several key steps:
- Patient Registration/Check-in: Front-desk staff collect and verify the patient's demographic information, medical history, and insurance details to ensure accuracy from the start.
- Insurance Verification: The provider verifies the patient's insurance coverage and eligibility for the specific services to be provided. This helps determine the patient's financial responsibility (copay, deductible, coinsurance) upfront.
- Medical Coding: The services provided during the patient encounter are translated into standardized alphanumeric codes using systems like CPT (Current Procedural Terminology) for procedures, ICD-10 (International Classification of Diseases) for diagnoses, and HCPCS (Healthcare Common Procedure Coding System) for supplies and other services.
- Charge Entry & Claim Submission: The assigned codes and associated fees are entered into a practice management system, compiled into a "superbill", and then submitted to the insurance company, typically electronically.
- Claim Adjudication: The insurance company reviews the claim to determine coverage eligibility and the amount they will pay. The claim may be accepted, denied (not covered by the plan), or rejected (errors needing correction and resubmission).
- Payment Posting: The payment received from the insurer is posted to the patient's account. The provider receives an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) detailing the payment, denial codes, and any remaining patient balance.
- Patient Billing & Collections: A statement is sent to the patient for any outstanding balance (e.g., deductibles, copays). The biller then follows up on unpaid claims and patient balances, which may involve setting up payment plans or, as a last resort, using a collection agency.
Medical Billing vs. Medical Coding
While often mentioned together, they are distinct functions:
- Medical Coding is the process of translating patient information from medical records into universal codes.
- Medical Billing involves using those codes to create and submit claims, track payments, resolve denials, and manage patient collections.
For Patients: Understanding Your Bill
Medical bills can be confusing. To understand your charges and rights:
- Review the EOB: Your health plan sends an EOB explaining costs, covered amounts, and what you owe. You should get this before a bill from the provider.
- Know Your Rights: The Centers for Medicare & Medicaid Services (CMS) provides resources on patient rights and protections, including how to dispute bills and the right to a "good faith estimate" for those without insurance.
- Contact Your Provider/Advocate: Talk to your provider's billing department or find a patient advocate for help resolving or negotiating medical bills.
Revenue Cycle Management (RCM) and ICD-10
- RCM is a continuous process: RCM tracks a patient’s journey from registration to final payment.
- ICD-10 is integral to RCM: Accurate ICD-10 coding is essential for proper billing, claim processing, and ultimately, getting paid for services rendered.
- Accurate coding prevents problems: Errors in coding can lead to claim denials, audits, and lost revenue.
Leukocytosis ICD 10
The main ICD-10 code for leukocytosis is D72.829, which is used for an unspecified elevated white blood cell count. This code is appropriate when the specific cause of the elevated white blood cells is unknown or not documented. When the specific type of leukocytosis is known, a more specific code from the D72.820-D72.828 range should be used.
Using the code D72.829
- When to use: Use D72.829 for "Elevated white blood cell count, unspecified" when lab results show a high white blood cell count but no further details are available.
- Importance: It is crucial to use the correct code for accurate medical billing and reimbursement.
- Documentation: Proper documentation is essential. This includes confirming the lab results and supporting the diagnosis with physician notes.
Using more specific codes
- Primary diagnosis: If leukocytosis is a secondary condition, the primary diagnosis should be the underlying cause (e.g., an infection or a malignancy).
- Specific types: A more specific code should be used if the type of leukocytosis is specified. For example, D72.820-D72.828 are used for specific types of elevated white blood cell counts.
Can medical bills affect your credit?
Yes, unpaid medical bills can affect your credit score if they go to a collection agency and meet certain criteria. The three major credit bureaus (Equifax, Experian, and TransUnion) have specific rules about when medical debt can appear on your credit report, which offer consumers some protection.
What happens if you don't pay hospital bill?
If you don't pay a hospital bill, you may face late fees, and the debt can be sent to a collections agency, which can damage your credit score and lead to further collection actions like wage garnishment or lawsuits. However, it's often possible to resolve the issue by checking for errors, negotiating a settlement, asking for financial assistance, or setting up a payment plan.
What is the icd 10 code for leukocytosis?
The ICD-10 code for unspecified leukocytosis is D72.829. This code is used for an elevated white blood cell count when the specific cause is not yet identified. Accurate documentation, including the specific WBC count and potential underlying causes like infection or stress, is crucial for proper billing and clinical management, according to RCM Experts and RevenueES.
About the Creator
khabe laim
I'm Khabe Laim, a blog writer covering diverse niches like medical billing, health & tech—crafting SEO-friendly, engaging, and informative content.






Comments
There are no comments for this story
Be the first to respond and start the conversation.