How does physical health relate to mental health, and why are both so important to manage?
physical health relate to mental health
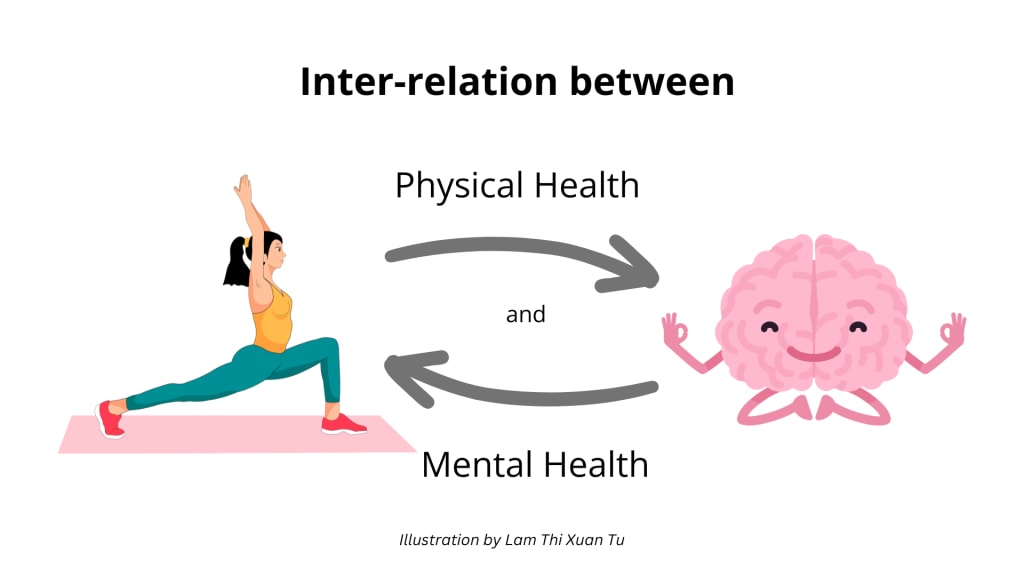
The interdependence between mental and physical health is profound. In the past, the medical community treated mind and body as different systems. Now, contemporary science and clinical practice affirm what many have experienced intuitively for a long time: physical and mental health are not separate but interconnected, and each affects the other profoundly. When one is afflicted, the other tends to follow—and when one heals, it can contribute to healing on a larger scale.
Understanding and respecting the dynamic relationship between emotional and physical well-being is essential for comprehensive health care. In this response, we’ll explore how mental and physical health are linked, how mental illness can manifest physically (and vice versa), and why addressing both holistically leads to better outcomes.
How Mental Health Impacts Physical Health
Mental disorders—e.g., depression, anxiety, trauma, and chronic stress—can have severe effects on the body. The brain, nervous system, hormones, and immune system are all involved in the stress response and management of feelings, so mental distress creates body changes.
1. Stress and the Body
Chronic stress increases cortisol and adrenaline levels, triggering a "fight-or-flight" response. While helpful in small amounts, chronic stress taxes nearly all body systems:
Cardiovascular: Increases likelihood of high blood pressure, heart disease, and stroke
Digestive: Can lead to ulcers, IBS (Irritable Bowel Syndrome), and appetite changes
Immune: Impairs immune function, leaving individuals more vulnerable to infection
Muscular/Skeletal: Creates chronic tension, headaches, and fatigue
Stress doesn't just feel bad—it wears the body down after a while.
2. Physical Health and Depression
Depression is often found to accompany sleeping problems, appetite changes, tiredness, and pain. It is also linked to inflammation and is now seen as a risk factor for cardiovascular disease and diabetes. Depressed individuals may also have behaviors (like smoking, drug abuse, or not exercising) that increase physical health risks.
3. Physical Symptoms and Anxiety Disorders
Anxiety can result in:
Irregular heartbeat and chest pain
Hyperventilation or shortness of breath
Gastrointestinal upset
Dizziness and fainting
Insomnia and muscle tension
These symptoms become chronic over time and can resemble or mimic physical disease.
How Mental Health Affects the Body
In the same way, mental health impacts the body, and physical disease tends to impact psychological and emotional functioning.
1. Mental Strain and Chronic Illness
Diseases like diabetes, cancer, arthritis, or heart disease are commonly coupled with:
Depression and hopelessness
Anxiety throughout the disease
Fear of disability or death
Social withdrawal and isolation
It is natural for patients who have chronic illnesses to experience disturbances in their mood, especially when their quality of life is impaired or if they feel that they have lost control over their bodies.
2. Neurological Conditions
Diseases of the brain and nervous system—such as multiple sclerosis, epilepsy, or Parkinson's disease—have a direct impact on thinking and mood. People with these diseases have very much larger rates of depression and anxiety.
3. Lifestyle and Mental Health
Basic habits of physical health like poor diet, inactivity, lack of sleep, and drug use can worsen mental illness. Conversely, starting to adopt good habits (even small changes) has tremendous positive effects on mental health.
Shared Risk Factors
Both mental and physical illness are brought on by a variety of factors:
Socioeconomic status: Low socioeconomic status, inappropriately inappropriate access to care, and ongoing stress are risk factors for both physical and mental illness.
Trauma and Adverse Childhood Experiences (ACEs): Early life trauma significantly enhances the risk of adult mental illness, coronary disease, obesity, and alcohol and drug addiction.
Genetics and family history: Several conditions share genetic components, i.e., depression and autoimmune diseases.
This mesh of influence highlights how important integrated care is.
Why Treating Both Matters
1. Improved Diagnosis and Outcomes
Those who are physically ill may not be tested for mental health, and vice versa. For example, someone with chronic pain may be suffering from unresolved depression, or someone with anxiety may be undergoing cardiac testing without probing psychological causes.
Integrated care models, where mind and body are treated simultaneously, lead to better diagnosis, compliance with treatment, and rates of recovery.
2. Enhanced Quality of Life
When physical and mental health are being treated simultaneously, patients have the advantage of:
Greater satisfaction with treatment
Increased ability to function in daily life
Reduced hospitalization
Extended life expectancy
Mental treatment for physical symptom management is improved, while physical symptom treatment allows for the recovery of emotional stability and motivation.
3. Reduced Stigma and Fragmentation
Recognizing the mind-body interaction demystifies mental illness by confirming their physical effects. It also reduces the tendency to "blame the patient" for symptoms that are not easily seen or measured.
Methods for Promoting Mental and Physical Health Together
Routine Mental Health Screening
Embed mental health testing within primary care settings, especially in patients with chronic disease.
Physical Activity
Exercise boosts mood, reduces anxiety, and improves sleep and cardiovascular functioning. 30 minutes a day walking can be revolutionary.
Mind and Body Nutrition
A balanced diet with omega-3 fatty acids, antioxidants, and fiber maximizes brain function and emotional well-being.
Sleep Hygiene
Sleep disorders affect both emotional and physical healing. Getting a top priority 7–9 hours of quality sleep improves all-around health.
Integrated Healthcare Teams
Interprofessional collaboration among general practitioners, psychiatrists, psychologists, and social workers offers holistic care.
Patient Education
Educate individuals on how their lifestyle practices, stress levels, and emotional responses are connected with physical health outcomes.
Mindfulness and Stress Reduction
Therapies like meditation, yoga, and breathing manage emotional tension as well as physical inflammation.
Physical and emotional health are not independent silos—each is a thread in the same fabric. Addressing one while neglecting the other puts an individual at risk for incomplete healing. True well-being arises from nurturing the whole person: mind, body, relationships, and life situation.
Seeing the link between physical and mental wellbeing gives people the power to take a more active and empathic response to self-care. It also challenges health systems to develop—so that nobody is left addressing symptoms in isolation, without acknowledging the deeper, interconnected realities of health.
If you or someone you know is struggling with physical or mental health problems, locating comprehensive, holistic care is one of the most important steps you can take towards a better quality of life.
For expert, compassionate mental healthcare, visit:
https://www.delhimindclinic.com/
https://www.craftcmsdeveloper.in/
You are welcome to call me if you wish to transform your Craft website or simply talk about your Craft project. I provide a no-obligation consultation!




Comments
There are no comments for this story
Be the first to respond and start the conversation.