Nanotech and the Future of Human Repair
Nanotechnology in Medicine
Nanotechnology – the manipulation of matter on an atomic and molecular scale – is emerging as a transformative force in medicine. This “bottom-up” engineering of materials at the nanometer scale offers unprecedented tools to repair and regenerate the human body. By designing devices and systems at the level of cells and molecules, scientists envision a future where our bodies can be healed at a cellular or even genetic level. In the not-too-distant future, human repair might mean using nanoscale robots to fix damaged organs, microscopic machines to ferry therapeutic agents to diseased cells, and gene-level editing to correct genetic defects. These technologies could revolutionize how we treat injuries, illnesses, and even aging itself. This article explores how nanotechnology is poised to enhance human repair, with a focus on targeted drug delivery, nanorobotics for internal medicine, genetic and cellular repair mechanisms, advances in tissue engineering, and the ethical considerations that accompany these innovations.
Nanotechnology in Medicine: An Overview
Nanomedicine – the application of nanotechnology in healthcare – encompasses a broad range of strategies. Nanoscale materials and devices can be engineered to have novel properties and functions that are not present in larger forms. For example, nanoparticles can be designed to be biocompatible (safe for use in the body) yet have unique interactions with biological systems. This makes them ideal for tasks like carrying drugs, delivering genetic material, or detecting disease at the earliest stages. Nanomedicine has already begun to make an impact in medical fields: it is improving the delivery of cancer treatments and imaging agents, developing better diagnostic tools, and even aiding in regenerative medicine approaches . In essence, nanotechnology provides the means to perform medical tasks at a resolution and scale that is much closer to the biological mechanisms of the body, opening up new possibilities for precision medicine and self-healing interventions.
One of the key advantages of nanomedicine is its ability to enhance drug delivery. Conventional drug therapies often suffer from low efficacy and side effects because drugs can’t target specific cells or tissues efficiently. Nanoparticles, however, can be tailored to carry drugs directly to the intended site – for instance, cancerous tumors – while sparing healthy tissue . They can also improve the solubility and stability of drugs, allowing more of the therapeutic agent to reach its target. As a result, smaller doses of medication can be used, reducing toxicity. Nanoscale drug carriers are already in use in clinical settings; for example, the chemotherapy drug Abraxane (which uses albumin-bound nanoparticle paclitaxel) is an FDA-approved nanomedicine that improves the delivery of a cancer drug to tumors. This and other nanotechnologies have shown that even today, nanomedicine can significantly improve treatment outcomes. The potential extends far beyond current applications, hinting at a future where the human body can be healed from within by nanoscale devices and therapies.
Targeted Drug Delivery and Cancer Therapy
Targeted drug delivery is a cornerstone of nanomedicine’s potential to repair and heal the body. In cancer treatment, for instance, conventional chemotherapy can kill cancer cells but also harms healthy cells, causing harsh side effects. Nanotechnology offers a way to deliver drugs precisely to cancerous tumors, sparing normal tissues. Researchers have developed various types of drug-loaded nanoparticles that can carry anti-cancer agents directly to tumors. These nanoparticles can be designed with surface coatings that allow them to evade the immune system and accumulate in tumors (a phenomenon known as the Enhanced Permeability and Retention effect) . Some nanoparticles are even functionalized with targeting ligands – molecules that bind to specific receptors on cancer cells – ensuring that the drug is delivered only to the cancerous cells. By doing so, the therapy is more effective and causes fewer side effects.
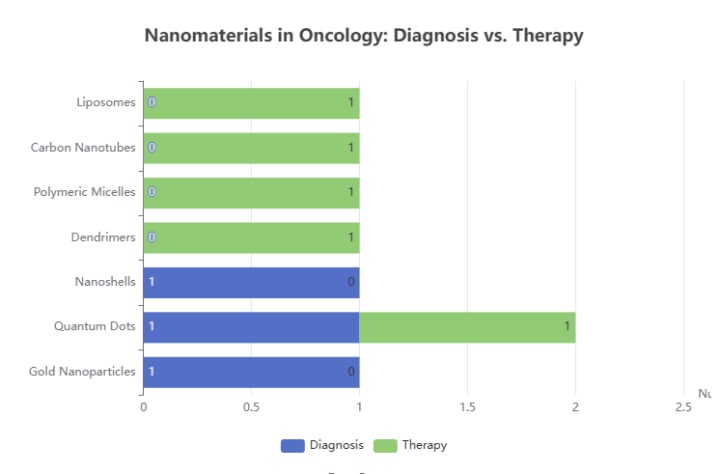
One prominent example of targeted drug delivery is the use of liposomes and polymer nanoparticles. Liposomes are microscopic lipid bubbles that can encapsulate drugs, and they have been used clinically for decades (e.g., Doxil for ovarian cancer). Polymer nanoparticles, made from biodegradable polymers, can similarly carry drugs and even respond to environmental cues (like pH changes) to release the drug at the right place and time. These carriers have made it possible to treat diseases that were previously untreatable or extremely difficult to treat. For example, certain anti-cancer drugs can now be delivered to tumors in a controlled manner, significantly improving outcomes. The chart below illustrates the wide range of nanomaterials used in both diagnosis and therapy, highlighting the versatility of nanotechnology in medicine.
Beyond cancer, targeted delivery is being explored for other conditions such as neurological disorders and cardiovascular diseases. In the future, one can imagine injecting a nanoparticle that specifically homes in on a tumor or a damaged organ, releases its therapeutic payload, and then either dissipates or is safely eliminated from the body. This level of precision could dramatically enhance the body’s ability to repair itself by treating diseases at the source with minimal collateral damage. Overall, targeted drug delivery – powered by nanotechnology – represents a paradigm shift in medical treatment, moving away from broad, systemic therapies toward finely tuned interventions that can heal specific problems with high efficiency.
Nanorobotics and Internal Medical Repair
A particularly exciting frontier in nanotechnology is nanorobotics, the development of tiny machines or robots that can operate within the body. Imagine microscopic robots that swim through the bloodstream, repairing cells, removing debris, or delivering medications directly to where they’re needed. While still largely in the research phase, nanorobots are a tantalizing vision of future medical repair. These nanoscale devices could be designed to perform tasks such as clearing blockages in blood vessels, sealing leaks in the heart or blood vessels, or targeting and destroying cancer cells from within. Because of their small size, they can navigate around cells and through tissues that are inaccessible to larger tools, effectively bringing medical care inside the body at a cellular level.
One major advantage of nanorobots is their ability to be programmable and autonomous. They can be equipped with sensors to detect specific conditions (like an abnormal chemical signal from a cancer cell or a drop in pH in an infected tissue) and then respond by performing a therapeutic action. For example, a nanorobot might carry a drug or a repair agent and release it when it encounters a cancer cell or a wound site. In cancer therapy, researchers have envisioned nanorobots that could home in on tumors, penetrate cancer cells, and deliver a lethal dose of medicine directly inside. They could even be designed to target specific genetic mutations or repair proteins inside cells. Such capabilities could turn cancer treatment from a one-size-fits-all approach into a personalized, on-demand repair process.
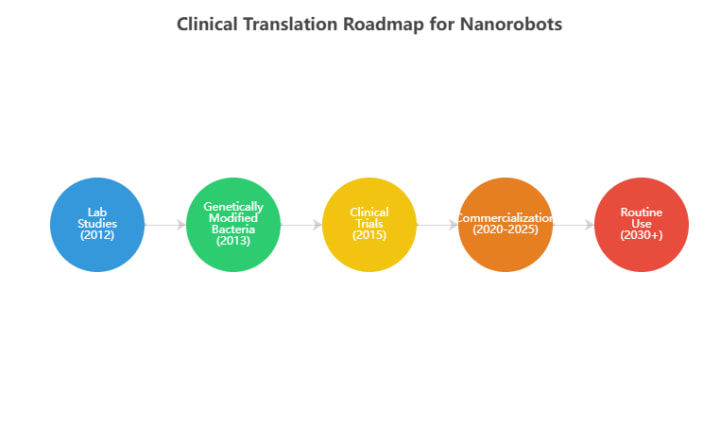
Another potential application of nanorobots is in diagnostics and monitoring. Tiny robots could continuously patrol the body, collecting data on health indicators and reporting back to a doctor. They might detect early signs of disease (like the presence of a few cancer cells or a pathogen) before symptoms appear, enabling proactive treatment. In the future, we might see “nanorobot doctors” that periodically examine the body’s systems and even make minor repairs on the spot – much like a mechanic might perform routine maintenance on a machine. While these scenarios sound like science fiction, there have been significant developments in the lab. Scientists have already created simple nanorobots that can move in a controlled manner, and research is ongoing to imbue them with more complex functions. The chart below provides a projected roadmap for the development and clinical translation of these nanorobots.
For instance, magnetic nanorobots that can be steered through the bloodstream using an external magnetic field have been tested in animal studies for targeted drug delivery. Likewise, DNA-based nanorobots that can change shape and carry cargo have shown promising results in delivering therapeutic genes to cells. In summary, nanorobotics offers a vision of medical repair that is truly inside-out: instead of relying on external treatments, the body could be equipped with tiny repair crews that go to work at the site of damage. While still years away from widespread use, these technologies represent a significant leap in the ability to heal the human body at a fundamental level.
Genetic and Cellular-Level Repair
Human repair at its most fundamental level involves fixing damage at the genetic and cellular level. Nanotechnology is now enabling new approaches to repair or replace faulty genes and cells. One area of focus is gene therapy – the delivery of genetic material to cells to treat or prevent disease. Traditional gene therapy often uses viruses or large vectors to carry DNA, but these can have limitations in terms of size and safety. Nanotechnology provides an alternative by creating tiny carriers (nanoparticles or nanofibers) that can ferry genes into cells. These nanocarriers can protect the genetic material from degradation and deliver it directly to the nucleus of target cells, where the genes can exert their therapeutic effect. This precision delivery is crucial for diseases caused by single gene defects, such as certain inherited disorders or cancer, where correcting the genetic code can be the ultimate form of repair.
Another aspect of cellular-level repair is using nanotechnology to enhance the body’s own repair mechanisms. For example, researchers are developing nano-sensors that can detect cellular stress or damage and then prompt the cell to repair itself. These nanosensors might be introduced into cells to monitor their environment; if a cell is stressed (say, due to oxidative damage or a malfunctioning protein), the sensor could trigger a repair pathway or even signal for help. Additionally, nanomaterials can be used to deliver proteins or enzymes that assist in cellular repair. For instance, nanoparticles carrying DNA repair enzymes could be used to fix genetic mutations or damaged DNA within cells. This could be revolutionary for treating genetic diseases or aging-related DNA damage, potentially allowing the body to repair itself at the molecular level.
Stem cell therapy – the use of stem cells to regenerate damaged tissues – is another area where nanotechnology plays a supportive role. Stem cells have the ability to differentiate into various cell types, making them valuable for tissue repair. However, getting stem cells to migrate to the right location and differentiate into the correct cell type can be challenging. Nanotechnology addresses this by creating scaffolds and matrices that guide stem cell behavior. Nanofibrous scaffolds can provide a structure that mimics the extracellular matrix (the network that supports cells in tissues), encouraging stem cells to grow and differentiate in a controlled manner. By using nanoscale materials, scientists can control the stiffness, porosity, and chemical properties of these scaffolds to influence how stem cells behave. This means that a damaged organ might one day be repaired by injecting stem cells along with a nanoscale scaffold that directs them to form new tissue exactly where it’s needed. In effect, the body’s own repair workforce (stem cells) is given a little help from nanotechnology to do its job more effectively.
Overall, advances in genetic and cellular-level repair through nanotechnology hold the promise of treating diseases at their root cause. Instead of merely managing symptoms, these technologies could enable the body to fix itself at the molecular level – whether that means correcting a genetic mutation, repairing a cell’s internal machinery, or regenerating an entire tissue. As research continues, we can expect to see therapies that not only treat disease but also help the body maintain itself, leading to a future where our genetic and cellular health is proactively managed and repaired.
Advances in Tissue Engineering and “Organs-on-Chips”
Tissue engineering is the field of creating functional tissues and even whole organs in the laboratory, which can then be used for transplantation or to study disease. Nanotechnology is significantly advancing tissue engineering by providing better tools to construct and guide tissue growth. One important application is the development of nanofibrous scaffolds for tissue regeneration. Traditional scaffolds (made of materials like collagen or synthetic polymers) have been used to support cell growth, but by using nanoscale fibers, scientists can create structures that more closely mimic the natural extracellular matrix in the body. Nanofibers have a large surface area and can be engineered to have specific surface chemistry, which influences how cells attach, grow, and differentiate. This can lead to the formation of tissues that are more biologically relevant and functional. For example, researchers have used nanofiber scaffolds to grow skin tissue, bone, and cartilage in the lab, with the goal of eventually transplanting these engineered tissues to patients.
Another exciting development is the creation of “organs-on-chips” – microfluidic devices that mimic the structure and function of an organ using living cells and nanotechnology. These chips are typically made of microscale channels and chambers, often lined with cells that form a tissue, and are covered with a flexible membrane (somewhat like a tiny human organ). By incorporating nanomaterials or nanoscale features, scientists can further refine these chips to better replicate the organ’s environment. For instance, a lung-on-a-chip might use a nanocomposite membrane that allows oxygen and gases to pass through much like alveolar tissue does. A heart-on-a-chip might have nanoscale structures that guide the alignment of heart muscle cells for more natural contraction. These organs-on-chips are not yet capable of full organ function, but they are invaluable tools for drug testing, disease modeling, and even tissue engineering. They allow researchers to study how organs respond to drugs or injuries in a controlled setting, and eventually, they could be used to generate transplantable tissues. The integration of nanotechnology ensures that these systems can be made extremely small and precise, accelerating progress in regenerative medicine.
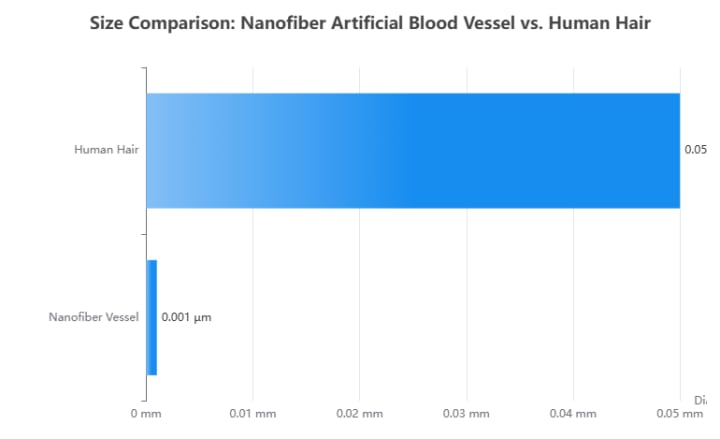
One notable example of nanotechnology in tissue engineering is the creation of artificial blood vessels. Researchers have used nanoscale materials to fabricate tiny blood vessel segments that can be implanted to bypass or replace damaged vessels. In one study, scientists developed a biomimetic blood vessel using an electrospinning technique to create an extremely thin nanofiber mesh, resulting in the world’s smallest artificial blood vessel (measuring only a few millimeters in diameter) . This nanofiber scaffold was populated with cells and showed great promise in animal studies, demonstrating that engineered blood vessels could function in the body. Such innovations are crucial for repairing cardiovascular damage and could eventually help patients who need organ transplants by providing replacement parts grown from their own cells. The following chart shows the size comparison of this breakthrough artificial blood vessel with a human hair, highlighting the remarkable scale of nanotechnology.
In summary, tissue engineering combined with nanotechnology is moving us closer to the reality of growing new body parts. Instead of relying solely on organ transplants or waiting for the body to heal itself, we may one day be able to create tissues and organs in the lab and implant them, much like we might replace a worn-out organ with a new one. This not only addresses the shortage of donor organs but also offers personalized solutions – tissues grown from a patient’s own cells, reducing the risk of rejection. The precision and control provided by nanotechnology in these processes ensure that the engineered tissues are as close to natural as possible, improving their functionality and long-term success in the body. As these technologies mature, we can expect to see significant advancements in regenerative medicine, enabling the body to repair and replace itself in ways that were once unimaginable.
The Future of Dental Implants with Nanotechnology
Nanotechnology has the potential to revolutionize the field of dentistry, particularly the future of dental implants. While traditional implants (typically made of titanium) already boast high success rates, they still face challenges such as infection, insufficient bone integration (osseointegration), and long-term durability. Nanotechnology addresses these issues at the molecular level, promising safer, stronger, and more effective implants.
One of the key advancements is the achievement of enhanced biocompatibility and faster osseointegration. Researchers are now coating implant surfaces with nanoscale textures that mimic the body’s natural bone structure. These nanostructured surfaces encourage bone cells (osteoblasts) to adhere, proliferate, and grow more effectively on the implant. For instance, nanocoatings made from bioactive materials such as calcium phosphate can accelerate bone formation, allowing the implant to bond with the jawbone more quickly and securely. This can significantly shorten healing times and improve implant success rates—especially in patients with low bone density.
Infection prevention is another critical application of nanotechnology in implantology. Infections around the implant (peri-implantitis) are one of the leading causes of implant failure. Nanotechnology helps reduce this risk by integrating nanoparticles with antibacterial properties—such as silver or zinc oxide—into the implant surface. These nanoparticles create a defense mechanism that inhibits bacterial growth and biofilm formation. Such “smart” antimicrobial surfaces minimize the risk of infection, thereby extending the implant’s lifespan.
Finally, nanotechnology also enhances the durability and mechanical performance of implants. Nanomaterials such as carbon nanotubes or graphene can be incorporated into composites to improve implant strength. This makes implants lighter yet more resilient, capable of withstanding higher chewing forces. Moreover, nanoscale sensors can be integrated into implants to monitor their condition, bone integration, or detect early signs of infection.
These advancements have the potential to transform dental implants from mere tooth replacement solutions into intelligent medical devices that actively support and monitor long-term oral health.
Ethical and Regulatory Considerations
While the potential of nanotechnology to enhance human repair is immense, it also raises important ethical and regulatory questions. The ability to manipulate matter at the molecular level brings with it new possibilities – and new risks – that society must carefully consider. One primary concern is safety and regulation. Nanoparticles and nanodevices introduced into the body could have unforeseen effects on health. For example, some nanoparticles might accumulate in organs or cross the blood-brain barrier, potentially causing toxicity or unintended side effects. Because nanomaterials can behave differently from larger materials, their long-term effects on humans are not yet fully understood. This lack of knowledge has led to calls for rigorous testing and oversight of nanomedical technologies before they are widely used in patients. Regulatory bodies are beginning to develop guidelines for nanotechnology in medicine, but the field is evolving quickly, making it challenging to keep up. Ensuring that these technologies are safe, effective, and properly regulated is crucial to gaining public trust and to prevent misuse.
Another ethical consideration is the potential for misuse of nanotechnology. Nanoscale devices could be misused in ways that pose risks to individuals or society. For instance, the same nanorobots or gene-editing tools that could heal the body could potentially be used as weapons or for unauthorized genetic modifications. The prospect of “nanoweapons” or the creation of bioterror agents using nanotechnology is a concern that has been raised in security circles. Additionally, if advanced medical nanotechnologies become available only to the wealthy, it could exacerbate existing inequalities in healthcare access. This has led to discussions about ethical use – ensuring that these technologies are developed and used in a way that benefits everyone, not just a privileged few. There is also the question of human enhancement: nanotech might not just be about healing disease, but also about improving normal human functions (for example, enhancing memory or physical performance). This blurs the line between therapy and enhancement, raising ethical debates about what it means to be human and whether such enhancements are fair or even desirable.
Ethical guidelines and regulations are still in the early stages for nanotechnology. International bodies and national governments are starting to address issues such as labeling of products containing nanomaterials, workplace safety for those handling nanomaterials, and oversight of experimental medical nanotechnologies. The consensus is that precaution is needed – proceeding with caution and transparency – until more is known about the long-term effects of nanotechnology on health and the environment. Public engagement and discussion are also important; ensuring that the development of these technologies is aligned with societal values and ethical principles is vital. In essence, the future of nanotechnology in human repair will depend not only on scientific innovation but also on how we, as a society, decide to regulate and govern these powerful tools. Responsible development and oversight will be key to harnessing the benefits of nanotech while minimizing its risks.
Challenges and Limitations
Despite the remarkable progress in nanotechnology and its promise for human repair, there are several challenges and limitations that must be addressed. One of the biggest challenges is scaling up these technologies from the laboratory to real-world applications. Many of the current advances are proof-of-concept studies conducted in controlled environments. Translating them into practical, reliable treatments for patients requires solving engineering and manufacturing issues. For example, producing large quantities of uniform nanoparticles or nanorobots that meet strict quality standards is technically difficult. Ensuring that these devices can be consistently produced and are safe in the body is a hurdle that needs significant research and development. Additionally, regulatory approval for novel nanomedical products is a lengthy and complex process, often requiring extensive clinical trials. This can delay the availability of new treatments and increase their cost.
Another limitation is the complexity of biological systems. The human body is incredibly complex and finely tuned, and nanoscale interventions must work within this complexity. A nanorobot or a nanoparticle must navigate through the bloodstream, avoid the immune system, and find the exact target without causing collateral damage. These tasks are not trivial and can lead to unpredictable outcomes. Moreover, biological processes can be dynamic – cells and tissues change over time – so a static nanodevice might not adapt well to these changes. Researchers are actively working on making nanotechnologies more adaptive and intelligent to handle these complexities. For instance, creating self-assembling nanoparticles that can adjust their behavior based on signals from the body is an area of active study.
Cost is also a practical consideration. Cutting-edge nanotechnologies can be very expensive to develop and produce. This could make them inaccessible to many patients, especially in healthcare systems with budget constraints. As with any new technology, it’s likely that costs will come down as the technology matures and is produced at scale, but initially, only those who can afford it might benefit. Ensuring that these innovations are affordable and widely accessible is an important challenge for the future of nanomedicine.
Finally, there are technological limitations to consider. Current nanorobots, for example, are relatively simple compared to the sophisticated robots in science fiction. They can perform basic tasks like carrying a payload or moving in a certain direction, but true autonomy and intelligence are still in the experimental stage. Overcoming these technical barriers – such as developing better power sources for nanorobots, improving their communication and coordination, and increasing their precision – is an ongoing challenge that will require interdisciplinary collaboration.
In summary, while the vision of using nanotechnology for human repair is compelling, there are practical and technical hurdles to overcome. The path from laboratory discovery to clinical application is long and challenging, but it is being actively pursued through research and innovation. With continued effort, many of these limitations can be addressed, bringing us closer to a future where nanotechnology truly enables widespread healing and self-repair. It’s important to recognize these challenges and to invest in research and development that will ensure these technologies are not only effective but also safe, affordable, and ethically sound as they move from the lab into our lives.
Conclusion
Nanotechnology stands at the forefront of a medical revolution that could fundamentally change how we repair and maintain the human body. By working at the atomic and molecular scale, scientists are creating tools that allow us to intervene in the body’s processes with unprecedented precision. From targeted drug delivery that heals diseases at their source, to nanorobots that could act as internal repair crews, to gene-level interventions that fix the very blueprint of life, the potential applications of nanotech in medicine are vast. We are on the cusp of a future where injuries might be repaired faster, diseases might be treated more effectively, and even aging might be slowed or reversed through nanoscale interventions. These technologies promise to make healthcare more personalized, more effective, and less invasive.
However, as we move forward, it’s crucial that we approach these innovations with careful consideration. Ethical guidelines, robust regulations, and rigorous scientific testing will be essential to ensure that nanotechnology is used safely and responsibly. The journey from visionary idea to routine medical practice is not without challenges – but the progress made so far is encouraging. Already, the field of nanomedicine has delivered tangible benefits, and researchers continue to push the boundaries of what’s possible. In the coming decades, we can expect to see nanotechnology integrated into everyday healthcare, helping to heal and protect the human body in ways that were once the stuff of science fiction. The future of human repair may well be written in nanoscale letters, offering a new era of health and longevity through the power of tiny machines and materials working in harmony with our biology.






Comments
There are no comments for this story
Be the first to respond and start the conversation.