Why Radiologist-Led Annotation Is the Foundation of Clinically Safe Medical AI
Why a radiologist's perspective – and high-quality labeled data – is essential for medical AI, and what developers should consider when selecting an annotation partner.
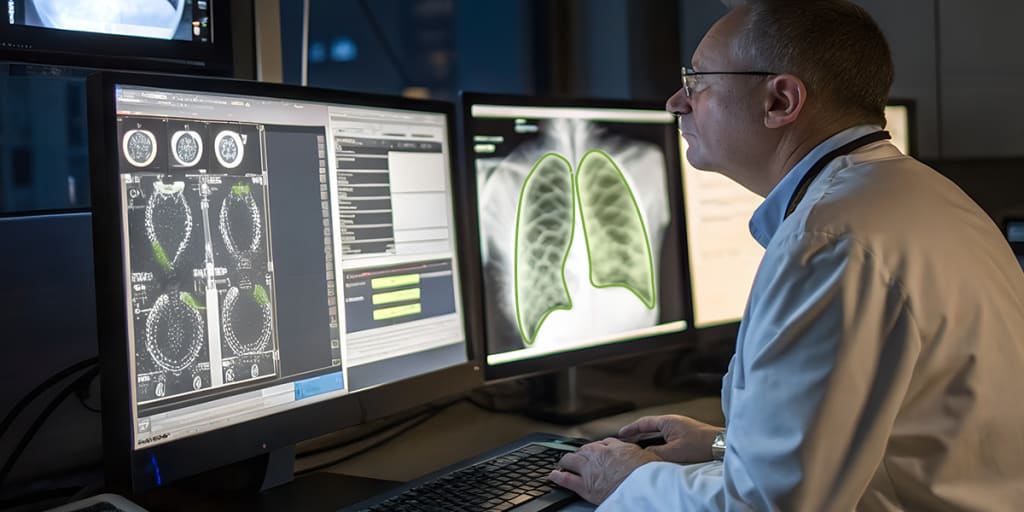
Artificial intelligence (AI) has shown significant potential in analyzing medical images and enhancing radiology workflows. However, in radiology, accuracy is not a luxury but a clinical necessity when models detect lesions in an MRI or quantify anatomical structures. Accuracy can be the difference between the right clinical decision and the wrong one. Annotation is an integral component of AI model development, and the only way to embed accuracy into these systems is by using high-quality labeled data curated, validated, and clinically guided by radiologists.
Data annotation is the process of transferring human knowledge to AI models by structuring and tagging digital data. In radiology, imaging modalities are annotated by domain experts to improve model performance. This article explores why a radiologist's perspective – and high-quality labeled data – is essential for medical AI, and what developers should consider when selecting an annotation partner.
Radiologist Experience on AI Annotation Quality
Annotated images are widely employed in medical AI to improve model performance. The medical image annotation process goes beyond marking or outlining anatomical structures or pathologies— and requires deep clinical expertise for accurate interpretation. Various factors, like variants, artifacts, acquisition parameters, and patient history context, influence how an image should be labeled. Therefore, it is inaccurate and unsafe to rely on a single annotator as the gold standard in preparing medical imaging data for AI models.
Radiologists and clinicians are essential across the entire data lifecycle: designing annotation schemas, overseeing the annotation workflow, training annotators, validating labels, and ensuring quality throughout.
Critical Roles of Clinicians and Radiologists Across the AI Training Data Pipeline
- Data Preparation
Radiologists play an important role in data preparation, particularly while sourcing imaging data from planned clinical studies. They create annotation guidelines based on a project’s clinical and technical requirements, determine the necessary data variability, including patient demographics, imaging modality, method of acquisition, and post-processing parameters – and ensure compliance with acquisition protocols and ethical considerations.
Once datasets are obtained, radiologists assess the suitability of each dataset for AI use, filter irrelevant or low-quality cases, and collaborate with statisticians, data scientists, and developers to prepare clean datasets. They also play a crucial role in documenting data curation for regulatory submissions (e.g., FDA).
- Choosing Annotation Tools
It is imperative to test annotation tools to ensure they meet annotators’ needs, support efficient and scalable workflows, and maintain regulatory compliance. There are plenty of tools in the market, but not all support medical workflows. Selecting the right tool can significantly boost annotation speed and quality.
Radiologists evaluate various aspects from a clinical standpoint, including evaluating usability, rendering accuracy, presets, and colormaps. They also review support for key factors such as:
• Imaging modalities (CT, MRI, X-ray, mammography)
• Workflow customization
• DICOM, NIfTI, and other format compatibility
• Data security, anonymisation, and compliance
• Quality-control features
• Licensing and deployment considerations
This helps ensure tools meet clinical, security, and regulatory requirements. Additionally, validated tools may also be required for FDA submission
- Annotation Planning
Radiologists determine which anatomies and pathologies need to be annotated based on project goals. They select the most relevant structures, identify negative classes essential for AI training, and provide clinical reasoning for the inclusion and exclusion of labels in the dataset. They work with data scientists to translate clinical requirements into technical annotation instructions and collaborate with technical teams to define the most appropriate approach to finalize annotation type – such as classification to tag an image as ‘normal’ or indicating a specific disease, segmentation to precisely outline the diseased region, or detection to draw a bounding box around the abnormality. Radiologists also guide the team on the best techniques to accurately label areas of interest across different imaging modalities, such as X-ray, CT, MRI, ultrasound, and PET.
- Data Annotations
As stated earlier, radiology images require advanced interpretation of ambiguous margins, subtle findings, and modality-specific artifacts. This makes radiologist oversight, both in supervising annotation teams and evaluating outputs, essential. Annotation in radiology can’t rely on a ‘single-annotator’ approach. Even often board-certified radiologists have varying diagnostic interpretations and levels of agreement. Therefore, it requires the same level of scientific rigor as the model training process. Subtle and complex findings – such as interpreting hazy areas in the lungs on a chest CT scan, identifying microcalcifications on mammography, or assessing changes in a lesion over multiple MRI scans – are not simple object-detection tasks. They are interpretation tasks that determine a model’s ability to make the correct clinical inference. Radiologists play a critical role in the annotation workflow – from guiding the process and training annotators to reviewing tricky or artifact-heavy images, providing feedback to technical teams, and serving as primary QA reviewers of internal annotations.
- Training of Annotators
Nuances, ambiguities, and intricacies in medical images require specialists with deep domain knowledge essential for training annotators on anatomy and pathology. Radiologists prepare detailed training documents with examples and illustrations, demonstrate common pitfalls based on internal pilot annotations, review test or pilot tasks from new labelers to validate accuracy, and provide ongoing training and feedback.
- Final Data Delivery Preparation
Radiologists assist technical teams in finalizing data for training and evaluating medical AI models by approving clinically validated, quality-checked annotated datasets and by ensuring proper segregation of data according to clinical relevance. They ensure that the data delivered for model development matches the intended clinical use.
Conclusion
Clinicians and radiologists play a central and irreplaceable role in building medical AI models that produce clinically accurate results. From planning and study design to defining annotation requirements and selecting the anatomies, pathologies, and negative classes that shape model behavior – their involvement spans every stage of the data lifecycle. Only radiologists can lay out accuracy standards, guide pilot studies, and ensure that every labeled sample reflects real-world clinical reasoning. Additionally, they ensure training datasets conform to ethical and privacy regulations by maintaining thorough documentation and offering final clinical sign-off on datasets. Their expertise reinforces clinical validity, reduces risk, and ensures that the AI models are trustworthy and ready for deployment in the real world.
About the Creator
Matthew McMullen
11+ Years Experience in machine learning and AI for collecting and providing the training data sets required for ML and AI development with quality testing and accuracy. Equipped with additional qualification in machine learning.






Comments
There are no comments for this story
Be the first to respond and start the conversation.