Prostatitis dampening sexual performance
Sex, Prostatitis and it's treatment.
Prostatitis, the inflammation of the prostate gland, is a common condition that affects men of all ages. Apart from causing urinary symptoms and pelvic pain, prostatitis can also have a significant impact on sexual performance. In this article, we will explore the connection between prostatitis and sexual function, the underlying causes, and the available treatment options to manage this condition effectively.
Understanding Prostatitis and Its Types
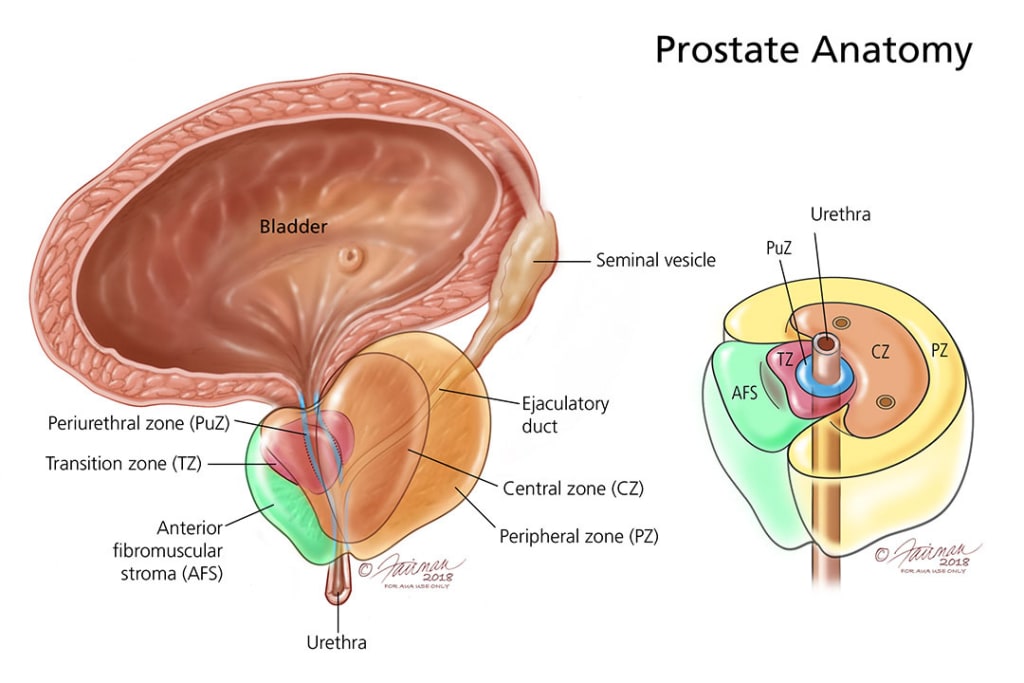
The prostate gland is a small walnut-shaped organ located below the bladder and in front of the rectum, surrounding the urethra. Its primary function is to produce seminal fluid, which nourishes and protects sperm. Prostatitis is classified into four types, each with distinct causes and symptoms:
Acute Bacterial Prostatitis: This type is caused by a bacterial infection and manifests as sudden and severe inflammation. It may result in fever, chills, frequent urination, painful urination, and difficulty emptying the bladder.
Chronic Bacterial Prostatitis: In contrast to acute bacterial prostatitis, this type involves recurrent or persistent bacterial infections. Symptoms may be less severe but can last for an extended period, leading to recurrent flare-ups of prostatitis.
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): This is the most common type and does not have an identifiable bacterial infection as its cause. Its symptoms can include pain or discomfort in the pelvic region, pain during ejaculation, and urinary difficulties.
Asymptomatic Inflammatory Prostatitis: As the name suggests, this type does not present any noticeable symptoms, and it is usually diagnosed incidentally during medical exams for other conditions.
Impact on Sexual Performance
Prostatitis can exert various effects on sexual performance, which can significantly impact the quality of life and intimate relationships. The severity of these issues may vary depending on the type of prostatitis and individual factors. Some common sexual problems associated with prostatitis include:
Erectile Dysfunction (ED): Erectile dysfunction can result from prostatitis due to several factors. The inflammation and pain in the pelvic region can lead to anxiety and stress, both of which are known psychological contributors to ED. Additionally, chronic inflammation may also affect blood flow to the penis, contributing to difficulties in achieving or maintaining an erection.
Pain During Ejaculation: Men with prostatitis may experience pain or discomfort during ejaculation. The inflammation of the prostate can lead to heightened sensitivity or irritation in the pelvic area, making ejaculation a painful experience.
Reduced Libido: Chronic pain and discomfort related to prostatitis can diminish a man's interest in sexual activity. The preoccupation with symptoms and the fear of exacerbating pain during sexual intercourse can lead to a reduced libido.
Premature Ejaculation (PE): Some men may develop premature ejaculation as a consequence of prostatitis. The discomfort or pain during sexual activity can lead to heightened anxiety, making it challenging to control ejaculation.
Psychological Impact: Apart from the physical symptoms, prostatitis can also take a toll on a man's emotional well-being. Feelings of frustration, embarrassment, and inadequacy may arise due to the inability to perform sexually as desired.
Treatment Options
Treatment for prostatitis depends on the type and underlying cause of the condition. A comprehensive approach that addresses both the physical and emotional aspects of the condition is essential. Some common treatment options include:
Antibiotics: For cases of acute bacterial prostatitis and chronic bacterial prostatitis, antibiotics are prescribed to target the underlying bacterial infection. It is crucial to complete the full course of antibiotics to ensure the infection is eradicated.
Alpha-Blockers: These medications are used to relax the muscles around the prostate and bladder, relieving urinary symptoms and reducing discomfort.
Pain Relievers: Over-the-counter pain medications or anti-inflammatory drugs may be recommended to manage pain and inflammation associated with prostatitis.
Warm Baths or Sitz Baths: Soaking in warm water can help alleviate pelvic pain and discomfort, promoting relaxation of the pelvic muscles.
Physical Therapy: Pelvic floor muscle exercises and other physical therapy techniques can help relieve symptoms and improve sexual function.
Lifestyle Changes: Adopting a healthy lifestyle can contribute to managing prostatitis symptoms. Reducing caffeine and alcohol consumption, managing stress, maintaining good hygiene, and staying physically active can be beneficial.
Psychological Support: Addressing the emotional impact of prostatitis is crucial. Seeking support from a therapist or counselor can help manage stress, anxiety, and feelings of inadequacy related to sexual performance issues.
Conclusion
Prostatitis can significantly impact sexual performance and overall well-being. Understanding the different types of prostatitis and their effects on sexual function is essential for seeking appropriate treatment. Timely intervention, along with a holistic approach that addresses physical and emotional aspects, can lead to better management of symptoms and an improved quality of life. If you suspect you have prostatitis or are experiencing sexual performance issues, consult a healthcare professional for accurate diagnosis and personalized treatment. Remember that seeking support and communicating openly with your partner about the condition can also play a vital role in coping with prostatitis-related challenges.
"Disclaimer: This article may contain affiliate links, so if you decide to buy a product through these links, I may earn a commission."





Comments
There are no comments for this story
Be the first to respond and start the conversation.