Chronic Prostatitis Leading to Azoospermia: Causes, Impact, and Treatment Options
Chronic Prostatitis Leading to Azoospermia
Chronic prostatitis is one of the most persistent urological conditions affecting men worldwide. While it often presents with urinary frequency, pelvic pain, or discomfort during ejaculation, one of its less discussed but deeply concerning complications is azoospermia, the complete absence of sperm in semen. For men hoping to conceive, this diagnosis can feel devastating. Understanding the link between chronic prostatitis and azoospermia is crucial for timely treatment and fertility preservation.
How Chronic Prostatitis Affects Male Fertility
The prostate gland plays a key role in nourishing and protecting sperm. When chronic inflammation sets in, the delicate balance of the male reproductive system can be disrupted:
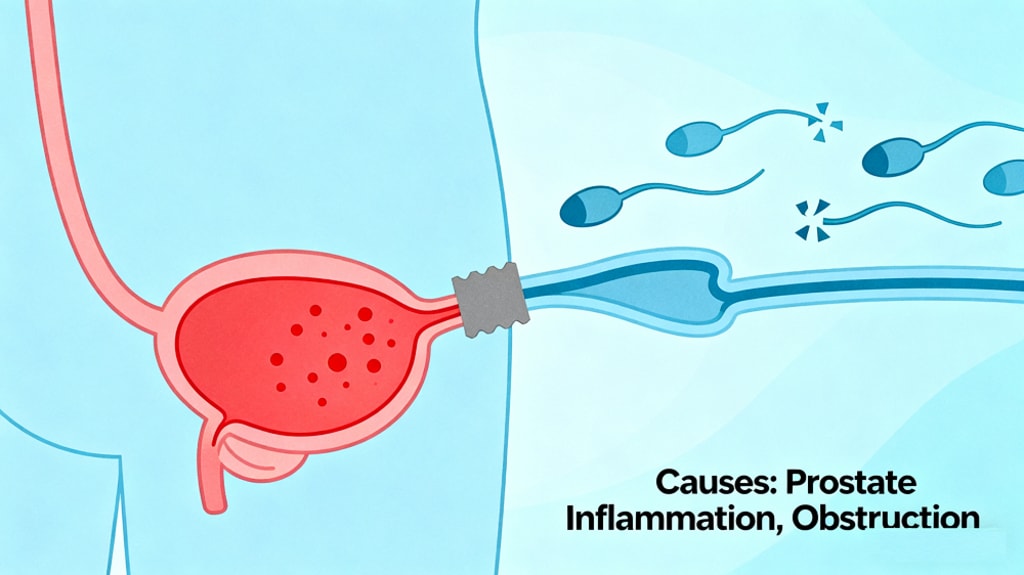
Obstruction of the Ejaculatory Ducts
Chronic inflammation may cause scarring or blockage within the ejaculatory ducts. This obstruction prevents sperm from mixing with seminal fluid, leading to obstructive azoospermia.
Direct Damage to Sperm Cells
Prolonged infection releases free radicals and inflammatory mediators that harm sperm DNA and decrease sperm viability, contributing to infertility.
Seminal Fluid Abnormalities
Chronic prostatitis alters pH levels, reduces zinc concentration, and increases white blood cell counts in semen—all of which negatively impact sperm survival.
Common Symptoms Indicating a Fertility Risk
Men with chronic prostatitis may notice:
Persistent pelvic or perineal pain
Painful ejaculation or reduced ejaculate volume
Hematospermia (blood in semen)
Long-standing difficulty conceiving despite regular unprotected intercourse
If these symptoms are present, especially with infertility concerns, a semen analysis should be performed promptly.
Diagnostic Evaluation
For men with suspected azoospermia linked to prostatitis, doctors may recommend:
Semen analysis (to confirm azoospermia and assess seminal fluid characteristics)
Transrectal ultrasound (TRUS) (to detect duct obstruction or calcifications)
Prostatic fluid culture (to identify bacterial causes)
Hormonal tests (to rule out non-obstructive causes)
Treatment Options
1. Antibiotic Therapy
When chronic bacterial prostatitis is diagnosed, antibiotics are usually the first-line treatment. However, antibiotic-resistant cases are increasingly common, which makes long-term management more complex.
2. Anti-inflammatory and Supportive Therapies
NSAIDs may relieve pain and reduce inflammation, but they do not resolve the underlying cause. Physical therapies, such as prostate massage or heat therapy, can also help reduce congestion.
3. Traditional Chinese Medicine: Diuretic and Anti-inflammatory Pill
For men with recurrent or antibiotic-resistant prostatitis, herbal therapies are gaining attention. The Diuretic and Anti-inflammatory Pill, a patented traditional Chinese medicine formula, has shown effectiveness in:
Clearing heat and toxins to combat chronic infection
Reducing swelling and relieving pelvic pain
Improving microcirculation, which helps restore prostate and seminal tract function
Promoting recovery of sperm production and ejaculatory duct health
Unlike antibiotics, this formula works holistically, aiming to regulate the body’s internal balance while addressing infection and inflammation.
4. Surgical Approaches
For men with confirmed duct obstruction, procedures such as transurethral resection of ejaculatory ducts (TURED) may be considered. Surgery can restore sperm passage in some cases.
Lifestyle and Self-Care for Better Fertility Outcomes
Balanced diet: Zinc-rich foods (oysters, pumpkin seeds) and antioxidants (berries, leafy greens) support sperm health.
Avoid smoking and alcohol: Both are linked to oxidative stress and impaired fertility.
Manage stress: Chronic stress worsens hormonal imbalance and sexual function.
Regular medical follow-up: Semen analysis every few months helps track recovery.
Prognosis and Fertility Outlook
Chronic prostatitis–induced azoospermia is a complex but not always permanent condition. With early diagnosis, targeted therapy, and supportive measures, many men can restore sperm production or explore assisted reproductive technologies. Importantly, men should not ignore ongoing prostatitis symptoms, as untreated inflammation can cause irreversible reproductive damage.
Conclusion
Chronic prostatitis leading to azoospermia is a serious yet manageable complication. Timely medical evaluation, appropriate therapies, and lifestyle adjustments can significantly improve fertility outcomes. For patients with antibiotic-resistant or recurrent cases, integrating Diuretic and Anti-inflammatory Pill offers a promising natural treatment option to restore prostate health and sperm function.
If you are struggling with prostatitis-related infertility, consult a urologist or reproductive specialist to develop a personalized treatment plan—because proactive care can make all the difference in preserving fertility.
About the Creator
George
I share practical, research-based insights on men's urogenital health—like prostatitis, orchitis, epididymitis, and male infertility, etc—to help men understand and improve their well-being.





Comments
There are no comments for this story
Be the first to respond and start the conversation.