What is depression and how can it be treated effectively?
depression
Depression is a serious mental health condition that affects how a person feels, thinks, and behaves. It goes far beyond occasional sadness or a temporary low mood. Depression can interfere with daily life, impact relationships, affect physical health, and reduce an individual’s overall sense of purpose and well-being. Understanding depression and how it can be treated is essential for anyone experiencing symptoms or supporting a loved one who may be struggling.
Understanding Depression
Depression, also known as major depressive disorder (MDD), is characterized by persistent sadness, hopelessness, and a loss of interest or pleasure in activities once enjoyed. It’s a complex condition that influences thoughts, emotions, and even physical health. People with depression may feel fatigued, find it hard to concentrate, experience changes in sleep and appetite, and have feelings of worthlessness or guilt. In severe cases, depression can lead to thoughts of self-harm or suicide.
It is important to recognize that depression is not a character flaw or a sign of personal weakness. It is a medical condition that results from a combination of biological, psychological, and environmental factors.
Common Symptoms of Depression
While everyone’s experience with depression may vary, common symptoms include:
Persistent sadness, emptiness, or tearfulness
Loss of interest in hobbies, work, or social activities
Fatigue or lack of energy
Difficulty concentrating or making decisions
Changes in appetite (eating too much or too little)
Sleep disturbances (insomnia or sleeping too much)
Feelings of guilt, worthlessness, or helplessness
Restlessness or slowed speech and movement
Physical aches or pains with no clear cause
Thoughts of death or suicide
To be diagnosed with major depressive disorder, these symptoms must be present for at least two weeks and cause significant distress or impairment in functioning.
Types of Depression
There are different types of depressive disorders, including:
Major Depressive Disorder (MDD): Intense symptoms that last for at least two weeks and interfere with daily life.
Persistent Depressive Disorder (Dysthymia): Chronic low mood that lasts for two years or more, often with less severe but longer-lasting symptoms.
Bipolar Depression: Occurs during the depressive phase of bipolar disorder, alternating with periods of mania or hypomania.
Postpartum Depression: Affects women after childbirth, involving intense sadness, fatigue, and anxiety.
Seasonal Affective Disorder (SAD): Depression that occurs during specific times of the year, usually in winter when there is less sunlight.
Atypical Depression: Features include mood reactivity, increased appetite, excessive sleep, and a heavy feeling in the limbs.
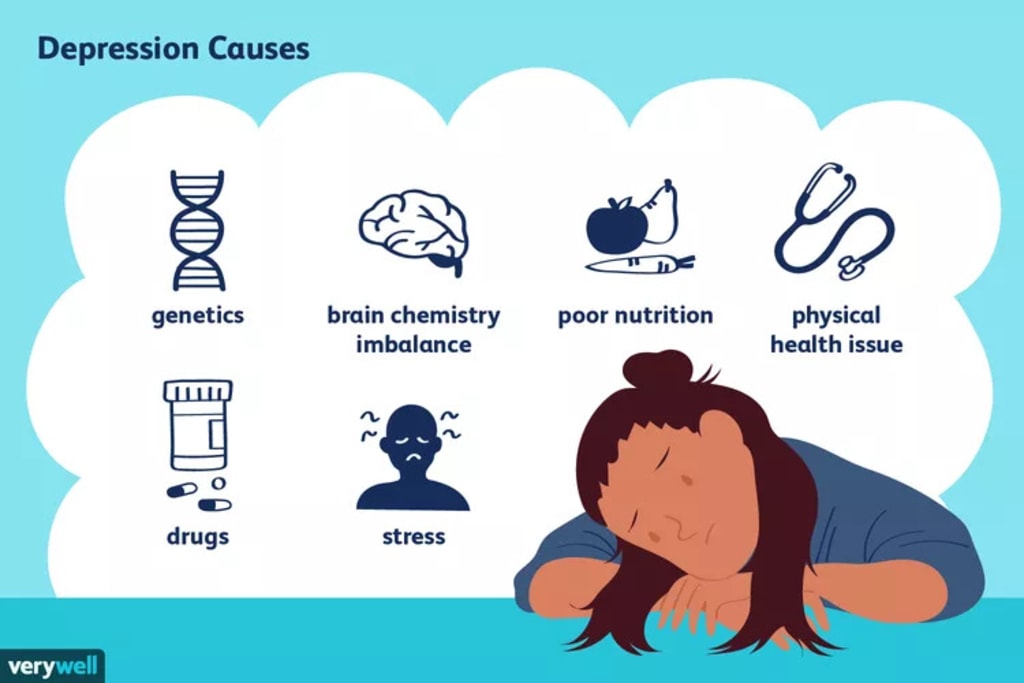
Causes and Risk Factors
Depression doesn’t have a single cause. Instead, it is influenced by a variety of interrelated factors:
Genetics: A family history of depression increases the risk, suggesting a hereditary component.
Brain Chemistry: Imbalances in neurotransmitters such as serotonin, norepinephrine, and dopamine are associated with depression.
Hormonal Changes: Hormonal fluctuations due to pregnancy, menopause, thyroid problems, or other health conditions can trigger depression.
Life Events: Trauma, loss of a loved one, relationship issues, financial problems, or chronic stress can be triggers.
Medical Conditions: Chronic illnesses like cancer, heart disease, or chronic pain often co-exist with depression.
Substance Abuse: Drug or alcohol misuse can lead to or worsen depression.
Personality Traits: People with low self-esteem, a pessimistic outlook, or high levels of self-criticism may be more vulnerable.
Diagnosis
A diagnosis of depression is made by a qualified mental health professional, such as a psychiatrist or clinical psychologist. The evaluation typically includes:
A detailed personal and family history
A discussion of symptoms, their duration, and their impact
Standardized screening tools like the PHQ-9 questionnaire
Medical tests to rule out other conditions, such as thyroid dysfunction or vitamin deficiencies
Early diagnosis is crucial in preventing symptoms from worsening and improving long-term outcomes.
Treatment Options
Depression is highly treatable, and many people recover completely or significantly improve with the right treatment approach. Most treatment plans combine multiple strategies to address both the psychological and physical aspects of the disorder.
1. Psychotherapy (Talk Therapy)
Psychotherapy is a cornerstone of depression treatment. Different types of therapy help individuals identify unhelpful thought patterns, manage stress, and build coping skills.
Cognitive Behavioral Therapy (CBT):
CBT helps individuals identify and challenge negative thoughts and beliefs, and replace them with healthier thinking patterns. It is one of the most effective treatments for depression.
Interpersonal Therapy (IPT):
IPT focuses on improving interpersonal relationships and social functioning. It helps patients navigate grief, role transitions, and unresolved conflicts.
Psychodynamic Therapy:
This approach explores unresolved past conflicts and how they impact current behavior and emotions.
Behavioral Activation:
Encourages individuals to engage in activities that bring joy and meaning, helping to counteract the withdrawal common in depression.
2. Medication
Antidepressants can help restore the chemical balance in the brain. They may take a few weeks to become fully effective and must be prescribed and monitored by a psychiatrist.
Common classes include:
Selective Serotonin Reuptake Inhibitors (SSRIs): Such as fluoxetine, sertraline, or escitalopram.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Like venlafaxine or duloxetine.
Tricyclic Antidepressants (TCAs): Older class, less commonly used due to side effects.
Monoamine Oxidase Inhibitors (MAOIs): Typically prescribed when other options fail.
Atypical Antidepressants: Such as bupropion or mirtazapine.
Finding the right medication may require trial and error. Patients should never stop medication abruptly and must follow their doctor’s guidance closely.
3. Lifestyle Modifications
Lifestyle changes can significantly improve mental health and act as a complementary treatment for depression.
Exercise:
Regular physical activity, such as walking or yoga, can boost endorphin levels and reduce depressive symptoms.
Diet:
A balanced diet rich in fruits, vegetables, lean proteins, and omega-3 fatty acids supports brain health.
Sleep Hygiene:
Maintaining a regular sleep schedule, avoiding screens before bed, and creating a restful environment can improve sleep and mood.
Stress Management:
Mindfulness, meditation, journaling, and breathing exercises help reduce stress and increase resilience.
Avoiding Alcohol and Drugs:
These substances can worsen depression and interfere with medications.
4. Social Support and Connection
Depression often leads to isolation, which can worsen symptoms. Staying connected with supportive friends, family members, or support groups can be healing.
Talking to others who have experienced depression can reduce stigma and feelings of loneliness. Group therapy or community programs can also offer encouragement and accountability.
5. Alternative and Complementary Therapies
While not a substitute for medical treatment, some individuals find benefit in complementary approaches such as:
Acupuncture
Massage therapy
Art or music therapy
Herbal supplements (e.g., St. John’s Wort, though this must be used cautiously under medical supervision)
6. Electroconvulsive Therapy (ECT)
In severe cases where other treatments fail, ECT may be considered. It involves electrical stimulation of the brain under anesthesia. ECT is safe and effective for treatment-resistant depression, particularly when suicidal risk is high.
Overcoming Stigma and Seeking Help
Stigma around mental health can prevent individuals from seeking help. Depression is a legitimate medical condition, not a personal failing. Education, awareness, and open conversations can help reduce stigma and encourage more people to seek the support they need.
Encouraging someone to talk to a professional, offering to accompany them to an appointment, or simply listening without judgment can make a big difference.
When to Seek Immediate Help
If someone expresses thoughts of suicide, hopelessness, or mentions a desire to harm themselves, it’s essential to seek immediate medical attention. Crisis hotlines, emergency psychiatric services, or local mental health facilities can provide urgent care.
In India, helplines like iCall (9152987821) or AASRA (91-9820466726) are available 24/7 for emotional support.
Conclusion
Depression is a challenging but treatable condition. With the right combination of therapy, medication, lifestyle changes, and support, most individuals can recover and lead fulfilling lives. Early intervention, consistent care, and compassion — from both professionals and loved ones — are essential in the healing process.
For compassionate psychiatric care, visit:
https://www.delhimindclinic.com/
For expert help with Craft CMS development or website needs, visit:
https://www.craftcmsdeveloper.in/
Feel free to reach out if you'd like to make changes to your Craft website or simply chat about your Craft project. I'm available for a free consultation!





Comments
There are no comments for this story
Be the first to respond and start the conversation.