PERIPHERAL ARTERY DISEASE
Lower limb arterial disease
I. SUMMARY:
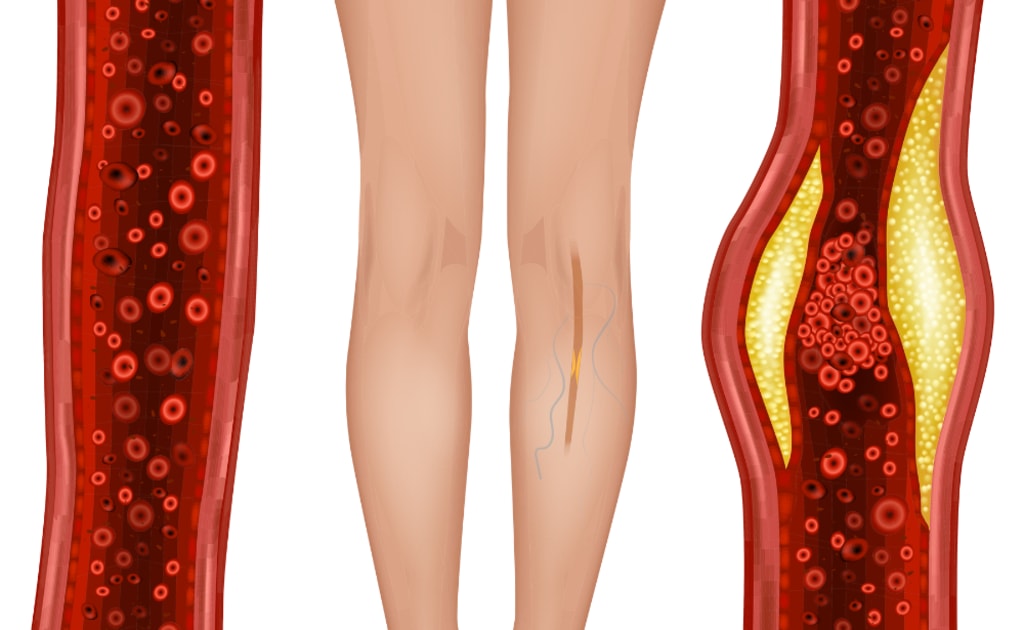
Peripheral artery disease (PAD) is a common condition in which the arteries become narrowed, reducing blood flow to the legs. This condition may also be called peripheral artery disease.
In PAD, the legs do not receive enough blood to meet their needs. This can cause leg pain when walking, also known as claudication, along with other symptoms.
PAD is often a sign of fatty plaque buildup in the arteries, a condition known as atherosclerosis.
Treatment for PAD includes regular exercise, maintaining a healthy diet, and not smoking or using tobacco products IN COMBINATION with medications and/or interventions, such as surgery, to re-open the blood vessels.
1. Alarming numbers:
PAD increases the risk of other cardiovascular diseases such as heart attack and stroke. Mortality rate is about 9%-15% within 1 year after diagnosis.
Smokers are 3 to 7 times more likely to develop lower limb arterial disease than non-smokers.
At the 2024 National Cardiovascular Science Conference, many cardiovascular experts also expressed concern about the trend of younger cardiovascular diseases, including lower limb arterial disease.
People with diabetes are 2-4 times more likely to develop lower limb arterial disease than normal people.
2. Symptoms of lower limb arterial disease
Lower limb arterial disease (PAD) may cause no symptoms or only mild symptoms. Common signs include:
• Leg pain when walking.
• Muscle pain or cramps in the arms or legs, usually in the calves.
• Muscle pain during exercise, relieved by rest.
• Cramping or pain in one or both hips, thighs, or calves after walking, climbing stairs, or doing other activities.
• A cold feeling in the lower leg or foot, especially when compared to the other side.
• Numbness or weakness in the leg.
• Weak or absent pulses in the leg or foot.
3. Characteristics of PAD Pain: PAD muscle pain can be:
• Mild to severe.
• Wakes you up at night.
• Makes it difficult to walk or exercise.
Even when resting or lying down, if the disease is severe. Other symptoms of PAD:
• Shiny skin on the legs.
• Changes in skin color on the legs.
• Slow-growing toenails.
• Ulcers on the toes, feet, or lower legs that do not heal.
• Hair loss or slower hair growth on the legs.
• Erectile dysfunction in men.
4. Causes of PAD:
PAD is often caused by a buildup of fat, cholesterol, and other substances in and on the walls of the arteries, causing atherosclerosis. This buildup is called plaque. When plaque forms, the arteries become narrowed, restricting blood flow. In PAD, plaque builds up mainly in the arteries of the legs. In addition to atherosclerosis, PAD can also be caused by less common conditions, such as:
• Vasculitis.
• Injury to the leg.
• Changes in the structure of muscles or ligaments that compress blood vessels.
• Exposure to radiation.
5. Complications of PAD
PAD can lead to serious complications, including:
🔴 Critical limb ischemia (CLI): When blood circulation to the limb is severely reduced, tissue can die from lack of oxygen. Typical symptoms include ulcers that do not heal on the hands or feet. If left untreated, amputation may be necessary.
🔴 Stroke & Heart Attack: Plaque not only narrows the arteries in the limbs, but can also affect the blood vessels of the heart and brain, increasing the risk of heart attack and stroke.
6. Preventing PAD
The best way to prevent leg pain from PAD is to live a healthy lifestyle. That means:
• Not smoking.
• Eating foods low in sugar, trans fats, and saturated fats.
• Exercising regularly
• Maintaining a healthy weight.
• Controlling blood pressure, cholesterol, and diabetes.
• Getting good sleep.
• Managing stress.
II. DIAGNOSIS
To diagnose PAD, your doctor will perform a physical exam and ask questions about your symptoms and medical history. If you have PAD, your pulse in the affected area may be weak or absent. To diagnose PAD or check for causes, commonly ordered tests include:
🔹 Blood tests: Check for factors that increase your risk of PAD, such as high cholesterol and high blood sugar.
🔹 Ankle-Brachial Index (ABI):
• This is a common test to diagnose PAD. Your doctor will measure and compare the blood pressure in your ankle and arm.
• You may be asked to walk on a treadmill, and your blood pressure readings will be taken before and immediately after exercise to assess the condition of your arteries while walking.
🔹 Doppler ultrasound of the leg or foot:
• Uses sound waves to create images of blood flow through the blood vessels in the legs and feet.
• Doppler ultrasound is especially useful in detecting narrowed or blocked arteries.
🔹 Angiography or CT scan of the blood vessels:
• This method uses contrast dye and imaging techniques to look for blockages in the arteries.
• The dye is injected into the blood vessels, helping to clarify the structure of the arteries on diagnostic images.
III. TREATMENT
Treatment for lower extremity arterial disease aims to:
• Control symptoms, especially leg pain, to help patients exercise more easily.
• Improve artery health, reducing the risk of heart attack, stroke, and other complications.
Treatment for PAD may include:
• Lifestyle changes.
• Medications.
• Surgery or endovascular intervention (if necessary).
1. Lifestyle changes
Lifestyle changes can help improve symptoms, especially in the early stages of the disease. Measures include:
✅ Quit smoking and nicotine products.
✅ Exercise regularly.
✅ Maintain a healthy diet.
2. Medication
If you have symptoms or complications of PAD, your doctor may prescribe the following medications:
🔹 Statins: Help lower “bad” cholesterol (LDL), limiting the formation of plaque in the arteries. These medications also help reduce the risk of heart attack and stroke.
🔹 Blood pressure medications:
• High blood pressure hardens and narrows the arteries, restricting blood flow.
• If you have high blood pressure, your doctor may prescribe medications to control it. Ask your doctor what blood pressure goals are right for you.
🔹 Diabetes medications:
• Diabetes increases your risk of PAD.
• Patients should monitor their blood sugar levels and follow their doctor's treatment instructions.
🔹 Anticoagulants:
• Reduced blood flow due to PAD can increase the risk of blood clots.
• Your doctor may prescribe aspirin or clopidogrel (Plavix) to prevent blood clots.
🔹 Leg pain medications:
• Cilostazol is a medication that can improve blood flow and help relieve leg pain when walking.
3. Surgery and intervention to treat PAD
In some cases, PAD or its symptoms may require surgery or a vascular intervention.
🔹 Thrombolytic therapy:
• If a blood clot is blocking an artery, your doctor may inject medication directly into the affected artery to dissolve the clot.
🔹 Angioplasty and stent placement:
• If a narrowed artery is causing leg pain due to PAD, this procedure can help improve blood flow.
• A small, balloon-tipped tube (catheter) is inserted into the artery. When the balloon is inflated, it helps widen the artery.
• To keep the artery from narrowing again, your doctor may place a small metal mesh frame (stent) inside the artery.
🔹 Bypass surgery:
• This creates a new path for blood flow around the blocked or severely narrowed artery.
• The surgeon uses a healthy blood vessel from another part of the body, connecting it to the lower part of the blocked artery.
• This improves blood flow to the muscles and reduces pain caused by PAD.
IV. HOME CARE
There are several changes you can make to help control lower extremity arterial disease (PAD). Here are some tips to help control PAD and prevent symptoms from getting worse:
1. Quit smoking and nicotine products
🚭 Don't smoke or use tobacco.
• Smoking damages your arteries and increases your risk of PAD.
• If you already have PAD, smoking can make it worse.
• If you need help quitting, ask your doctor about effective ways to quit.
2. Exercise regularly
🏃♂️ Exercise is an important part of treating PAD.
• Physical activity improves blood flow to your arms and legs, reducing PAD symptoms.
• Doctors often recommend a supervised exercise program for people with PAD.
• This program combines exercise and education and can help increase the distance you can walk without pain.
3. Proper nutrition
🥦 Eat a healthy diet to protect your arteries.
• Prioritize fruits, vegetables, and whole grains.
• Limit sugar, salt, and saturated fat.
4. Check the label
💊 Check the ingredients on over-the-counter medications.
• Some decongestants (such as Advil Cold and Sinus, Claritin D, etc.) contain pseudoephedrine, which can constrict blood vessels and make PAD symptoms worse.
5. Adjust your leg position while sleeping
🛏 Adjusting your leg position may help relieve pain.
• Raising the head of your bed a few inches may improve blood flow.
• Keeping your legs below heart level often helps relieve pain.
• Some people find that hanging your legs off the edge of the bed or walking around can temporarily relieve pain.
6. Take care of your feet
👣 PAD reduces blood circulation, making it harder for cuts and sores on your feet to heal, especially if you also have diabetes.
How to take care of your feet properly:
✅ Wash your feet daily and dry them thoroughly.
✅ Moisturize your feet to prevent cracking, but do not apply cream between your toes (as this can increase the risk of fungal infections).
✅ Wear thick, dry socks and well-fitting shoes.
✅ Treat fungal infections of the feet such as athlete’s foot early.
✅ Be careful when trimming your toenails.
✅ Check your feet daily for cuts, ulcers, or other injuries. If you notice anything unusual, see your doctor.
✅ Consult a podiatrist to treat foot conditions such as calluses, corns, or toe deformities.
About the Creator
Truong Nguyen Hung
I am Truong Nguyen, a specialist in Thoracic and Vascular Surgery. With many years of experience, I am committed to providing the most accurate, and useful medical information. Join me in exploring important knowledge to protect the health,






Comments (1)
Well and good writting for Peripheral artery disease (PAD).