Diagnostic Imaging Within Pathology
Different Imaging and How They Show Up in Pathology
Where does the embolus usually start, and how does the embolism travel to the lungs?What happens to the lungs and heart when there is a pulmonary embolism? In your current work environment (Diagnostic, CT, MRI, Radiation Therapy, Ultrasound, Nuclear Medicine, Interventional Radiology/Cath Lab, etc.), what exams do you commonly perform on patients with pulmonary embolus?What does an embolism or a thrombus look like in your modality?
I am a radiology technologist and I am taking this class as part of my requirements to achieve my Bachelors in Radiologic Sciences. I have been an imaging professional for the last three and a half years, and have been crossed trained in both computed tomography and magnetic resonance imaging. I am currently working in a freestanding emergency room as a diagnostic x-ray/ CT tech.
A pulmonary embolism is usually defined as a partial or complete occlusion of a pulmonary branch. This is usually the cause of a plevlic or leg thrombosis. Pulmonary embolism and deep vein thrombosis are different pathologies that usually have the same underlying event, which is venous thromboembolism.(Schellhaaß et al., 2010)
With pulmonary embolism being an obstruction of the pulmonary circulation system, which happens when a clot has broken off and moves through out the blood system until is has caused the obstruction with in the pulmonary system.
This clot causes the heart to try and pump fast and work harder to overcome the clot. The heart working this hard for an extended period of time will cause the heart to weaken and could eventually become enlarged. Which will lead the heart failure.
I work mostly within computed tomography so in cases of pulmonary embolism we will either do a plain Chest CT or usually a Chest CT with PE protocol, which uses contrast to enhance the veins.
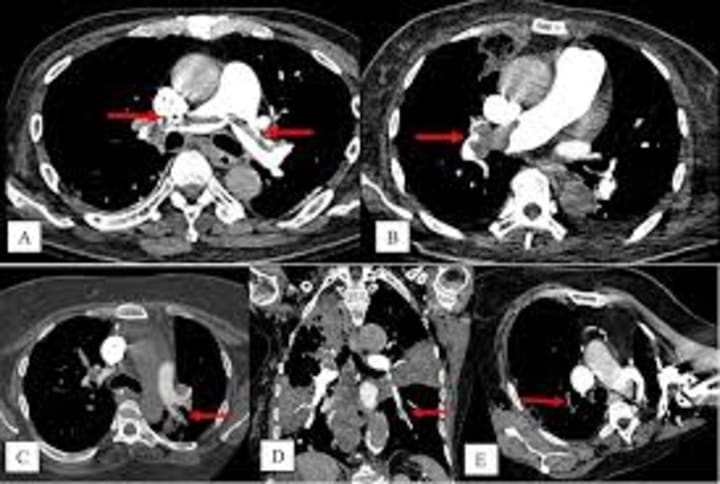
The image above shows how the obstruction would appear within a CT Chest PE protocol image.
______________________________________________
Gastrointestinal
Pick a gastrointestinal pathology discussed in the chapter and describe an imaging examination you perform to diagnose that pathology in your current work environment. Describe the radiographic features of the pathology on the examination you selected. What about the pathophysiology of the selected pathology makes it diagnosable on your exam? Convince others in your class that the test you are performing is the best test to diagnose the selected gastrointestinal pathology.
When a patient comes into the emergency room complaining of abdomen pain depending on the the area that they are complaining about, will depend on what the doctor believes the issue can be. Usually the exam that will get done will be a computed tomography of the abdomen. Now depending on the type of pain will depend on wither or not contrast is used. In the case of suspected pancreatitis, contrast will usually be used in these cases.
An intravenous contrasted computed tomography exam of the abdomen, allows the for the vessels and vein to be enhanced. When a patient has suspected pancreatitis using IV contrast with the scan can show and enlarged and or irregular outlined shaped of the pancreas.
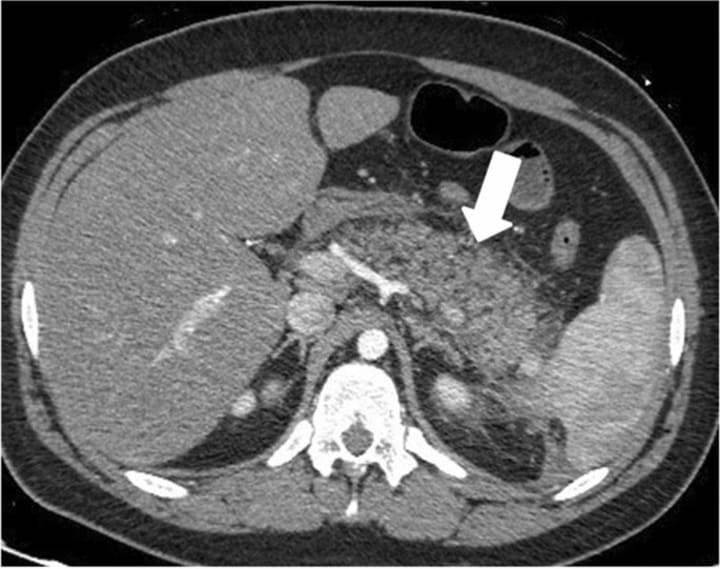
When trying to diagnosis pancreatitis it is largely accepted to use IV enhanced CT scan. You can use other imaging modalities however when it comes to keeping up with staging and any possible necrosis and or fluid collections that could happen. It is the most convent and detailed imaging for this type of disease.
Schellhaaß, A., Walther, A., Konstantinides, S., & Böttiger, B. W. (2010). The diagnosis and treatment of acute pulmonary embolism. Deutsches Ärzteblatt International. https://doi.org/10.3238/arztebl.2010.0589
___________________________________________________
Stroke
You can discuss stroke and its effects on the neurologic system. What are the causes of stroke or cerebral vascular accident (CVA)? What factors determines the long-term effects the CVA? What are the physical signs that a patient maybe having a stroke? How is CVA imaged in your modality? What are your hospital’s protocols for patients experiencing a CVA? (Stroke protocol, or stroke alert protocol, door to thrombolytic time protocol, etc.)
"Stroke is the fourth leading cause of death in the United States and the second most common cause of death worldwide; stroke is also the leading cause of long-term disability worldwide,"(Dorrance & Fink, 2015). There are two main types of stroke or cerebrovascular accidents, which occur when blood flow to the brain has been interrupted; by either a blockage, which is a type a ischemic stroke, or a rupture of a blood vessel, which is a type of hemorrhagic stroke. These are what leads to brain damage.
There are many factors that can affect what the long term effects of a cerebrovascular accident/stroke. One of the main factors is the location and the severity of the attack. Another factor is the amount of brain matter that was affected by the stroke. The age of the patient, the younger the patient the better the prognosis, and any pre-existing health conditions and how serious they take their rehabilitation efforts.
The physical signs of a patient is having a stroke is numbness or weakness, this is usually in one side of the body. It is usually in the face, arms, and/ or legs. This can also be companied by facial drooping usually on the numb or weak side of the body. A patient may also experience slurred speech and have vision changes, for example doubled or blurred vision. Other possible signs of stroke is loss of balance, confusion or difficult thinking, and severe intense headache.
I am currently working in a freestanding emergency room as a diagnostic x-ray/ CT tech. At my faculty we are not set up to handle the treatment of a stroke/cerebrovascular accident. If a patient comes in with a suspected stroke after the doctor has examined them. Then we immediately take them to CT and do a scan of the head, while the nurses are contacting hospital and EMS to transfer them and make sure they are able to get the medical attention they need.
Dorrance, A. M., & Fink, G. (2015). Effects of stroke on the autonomic nervous system. Comprehensive Physiology, 1241–1263. https://doi.org/10.1002/cphy.c140016
__________________________________________________
Visualize a disease process that could inhibit the sensory pathway. How would it affect the person? Which imaging modality might be useful in demonstrating the pathology.
Cerebral Palsy
Cerebral palsy is a health condition characterized by a neurological condition that affects the brain and nervous system. Cerebral palsy is a condition that could inhibit the sensory pathway. Cerebral palsy is the most common motor disability in children. Cerebral means having to do with the brain; palsy means weakness or problems with movement.
Cerebral palsy can manifest in a variety of ways and be expressed in a wide range of medical problems. It mainly involves movement and usually involves balance issues and sensory deficits. Research has also shown that cerebral palsy can be linked to blindness, hearing loss, and scoliosis due to the progression of muscle spasms.

Magnetic resonance imaging and ultrasounds are the main imaging methods used to diagnose cerebral palsy. The ultrasounds can be perinatal, and the magnetic resonance imaging can be done postnatally to help identify any birth injuries or abnormalities.
Neuroimaging may be obtained if perinatal imaging studies, such as fetal anatomy surveys or newborn transcranial ultrasonography, do not show a cause for the clinical findings. Magnetic resonance imaging is the recommended imaging modality and is preferable to computed tomography, given its higher specificity for identifying intracranial abnormalities.

Accardo, J., Kammann, H., & Hoon Jr, A. H. (2004). Neuroimaging in cerebral palsy. The Journal of Pediatrics, 145(2). https://doi.org/10.1016/j.jpeds.2004.05.018
Cerebral palsy: Living with paralysis: Reeve Foundation. Christopher & Dana Reeve Foundation. (2024, April 4). https://www.christopherreeve.org/todays-care/living-with-paralysis/health/causes-of-paralysis/cerebral-palsy/
Papadelis, C., Butler, E. E., Rubenstein, M., Sun, L., Zollei, L., Nimec, D., Snyder, B., & Grant, P. E. (2018). Reorganization of the somatosensory cortex in hemiplegic cerebral palsy associated with impaired sensory tracts. NeuroImage: Clinical, 17, 198–212. https://doi.org/10.1016/j.nicl.2017.10.021
Vitrikas, K., Dalton, H., & Breish, D. (2020, February 15). Cerebral palsy: An overview. American Family Physician. https://www.aafp.org/pubs/afp/issues/2020/0215/p213.html
About the Creator
Nyx Esmeray
I work as a Radiology Technologist, I have discovered a love of bullet journaling and rediscovered my love of books. I am trying to learn more about finances and discovering my spirituality.
https://linktr.ee/nyxesmeray






Comments (1)
Hey, just wanna let you know that this is more suitable to be posted in the Longevity community 😊