Healthcare and Pharmaceutical Software Development
Crash course on building apps for pharmacies and healthcare. Various sorts of software, essential features, user instructions, etc.

Many new entrepreneurs view healthcare software development as a daunting field—and for good reason. It’s shaped by strict legal frameworks, stringent data privacy requirements, outdated hospital IT infrastructures, and an immense sense of accountability. After all, when lives rely on your application functioning flawlessly, the stakes are far higher than launching a simple meal-delivery service.
That said, this is also where you can create genuine, meaningful change. Imagine an app that helps your grandmother remember to take her daily medication—real-world impact like that is possible. And you don’t need to be a physician or a legal expert in healthcare regulation to build something useful.
In this guide, we’ll dive into pharmaceutical IT solutions. You’ll learn about the development lifecycle, commonly used technology stacks, estimated costs, and other foundational insights—so you’ll know what truly works and what’s better left on the drawing board.
What Exactly Is Healthcare Software Development?
Put simply, when a patient visits a clinic—gets examined, undergoes tests, or is admitted—their personal details, diagnoses, lab reports, billing info, and more all need to be recorded and managed. Healthcare software exists to handle precisely that.
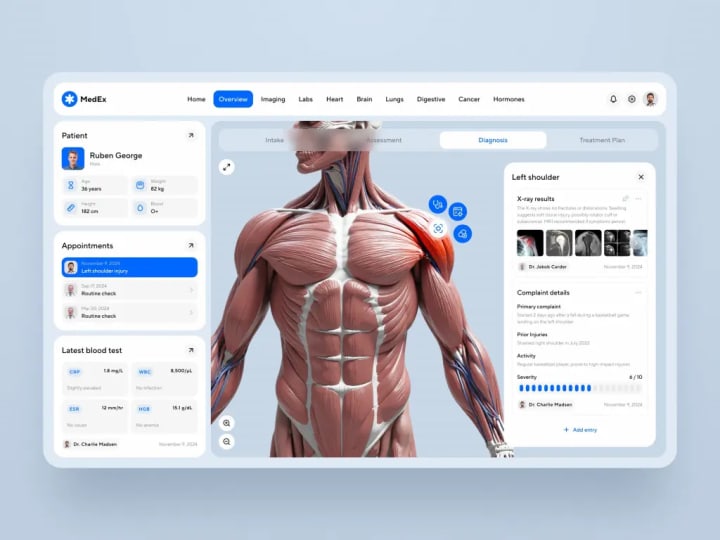
It’s an interconnected suite of digital tools designed to support clinicians, nurses, hospitals, insurers, and even patients in delivering and managing care. Common examples include electronic health records (EHRs), telehealth platforms, patient-facing portals, scheduling systems, and apps that remotely monitor chronic conditions.
The overarching goal? Streamline care delivery, enhance safety, and eliminate reliance on paper-based workflows. Because of the sensitive nature of health data, these systems must be trustworthy, resilient—and compliant with regulations like HIPAA (in the U.S.), GDPR (for EU data), and various regional standards. We’ll explore compliance in more detail shortly.

What Does Pharmaceutical Software Development Involve?
Unlike clinical care tools, pharma-focused software supports the journey of a drug—from research and manufacturing to distribution and post-market surveillance.
Think of platforms that manage clinical trial data: tracking which participant received what dose, when, and what side effects emerged. Or systems that ensure end-to-end traceability of medications—from production facilities to retail pharmacies. Other examples include Manufacturing Execution Systems (MES), pharmacovigilance tools that monitor adverse drug reactions, and AI-driven platforms that help scientists simulate molecular interactions.
Regulatory demands here are equally rigorous. Standards like FDA 21 CFR Part 11 (governing electronic records), GxP guidelines, and comprehensive audit trails—capturing every user action—are mandatory. Deployment isn’t a “push and hope” scenario; rigorous documentation, validation, and repeated testing are essential.
Key Distinctions—and Overlaps—Between Healthcare and Pharma Software
Healthcare software is patient- and provider-centric, focusing on the efficient delivery of care. It’s often real-time, interactive, and built for end-users—whether that’s a doctor reviewing lab results or a patient booking an appointment.
Pharma IT, by contrast, leans into research, quality control, and regulatory compliance. It’s less about immediate patient interaction and more about ensuring drug safety, efficacy, and supply chain integrity.
Despite these differences, the two domains increasingly converge. Consider personalized medicine: identifying eligible patients for a targeted therapy requires EHR data, while producing and tracking that therapy relies on pharma systems. Both sides also face significant interoperability challenges—getting hospital EHRs to communicate seamlessly with clinical trial platforms often demands sophisticated middleware.
Security is equally critical in both realms. A breach in healthcare exposes private medical histories; in pharma, it could leak proprietary research worth millions.
Market Landscape
Just as people now order groceries or clothes online, digital pharmacies are becoming mainstream. In fact, over half of U.S. adults have used an online pharmacy. Post-pandemic digital habits have stuck, especially among younger users who expect seamless, app-based experiences—why wait in line when a prescription refill is just two taps away?
U.S. e-pharmacy sales have surpassed $100 billion, and that’s before broader integration of telehealth-to-prescription models gains full regulatory approval. Globally, emerging markets are rapidly adopting digital drug delivery, particularly in regions with limited physical pharmacy access.
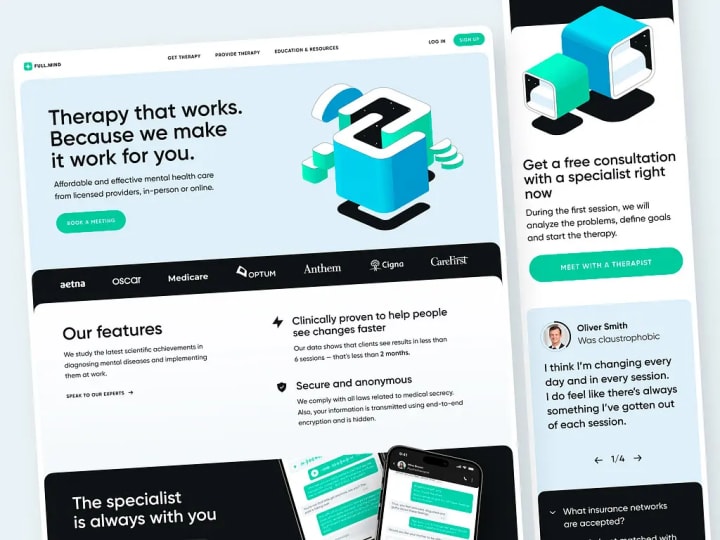
Popular areas for custom health software include telemedicine (e.g., Teladoc), mental wellness (e.g., Calm), fitness tracking (e.g., Fitbit), and medication adherence (e.g., Medisafe). Studying these can reveal both opportunities and pitfalls.
Types of Pharmacy Applications
Marketplace Models
These function like food delivery apps—but for medications. Users compare prices across local pharmacies, choose delivery options, and have prescriptions dropped at their door. Companies like Capsule pioneered this approach. Success hinges on dense urban logistics, real-time inventory sync, and robust APIs from partner pharmacies. Handling controlled substances adds complexity, requiring enhanced verification and compliance layers.
Direct-to-Consumer (DTC) Pharmacies
Here, you operate the pharmacy yourself—handling sourcing, fulfillment, and support. Examples include Blink Health and K Health’s prescription service. While this demands more operational oversight, it offers better margins and tighter control over user experience. These platforms often integrate telehealth: a virtual consultation leads directly to a digital prescription and checkout—within a single flow.
Technically, they require e-prescribing gateways, insurance eligibility checks, and payment systems that support FSA/HSA cards—all backed by detailed audit trails for every prescription change.
Chain Management Systems
Large pharmacy chains (CVS, Walgreens, Boots) rely on internal software for inventory, staffing, and inter-store logistics—many of which are outdated. Modern chain management apps centralize operations: offering real-time stock visibility, AI-driven reorder suggestions, and alerts for expiring inventory. Though not consumer-facing, they solve critical operational pain points and often integrate deeply with ERP and POS systems, fostering long-term vendor relationships.
Clinical Reference Tools
Not all pharmacy apps sell medication. Tools like Epocrates, Lexicomp, or Medscape serve as digital handbooks for professionals. Doctors check drug interactions; nurses verify drip rates; pharmacists confirm substitutions. These are typically monetized via subscriptions or ads—and accuracy is paramount, as errors carry legal liability.
Building one requires access to authoritative medical databases, frequent content updates, offline functionality, and a UI optimized for speed—because during emergencies, every second counts.
Why Invest in Custom Pharmacy Software?
Off-the-shelf solutions exist, but they rarely differentiate your brand or scale with your ambitions. Custom development offers distinct advantages:
- Revenue Growth & Market Reach: A well-designed app attracts new users—especially digitally native generations—and serves existing ones better. It transcends geography: a patient in a rural area can now access specialty medications they couldn’t before. Features like auto-refills, loyalty rewards, or OTC bundles create recurring revenue.
- Enhanced Patient Engagement : Traditional pharmacy experiences are often frustrating: long waits, unclear instructions, unexpected costs. An intuitive app can transform this—offering chat support with real pharmacists, adherence reminders, and proactive notifications. With user consent, anonymized data can reveal trends (e.g., frequent co-use of sleep and anxiety meds), enabling personalized wellness bundles.
- Operational Efficiency : Automation reduces manual labor: inventory tracking, document handling, audit prep—all become faster and less error-prone. AI can flag potential prescription errors before they reach the patient. Even simple features like in-app ID uploads save staff hours daily, lowering administrative overhead.
- Competitive Edge : Generic apps feel impersonal. A custom solution—featuring a sleek interface, deep EHR integration, or wearable-based reminders—stands out. When price and product are equal, user experience wins.

Essential Features for Pharmacy & Healthcare Apps
- Secure Authentication : Medical data demands more than basic login credentials. Implement multi-factor authentication (MFA), encrypted session tokens, auto-logout after inactivity, and role-based access (e.g., pharmacists vs. couriers). Avoid relying solely on third-party OAuth for sensitive operations.
- Prescription Management : This is the app’s backbone. Users should easily view active meds, request refills with one tap, track status (pending, shipped), and receive low-stock alerts. Smart features—like suggesting refills based on usage—add value but must clearly explain delays due to insurance or physician approval.
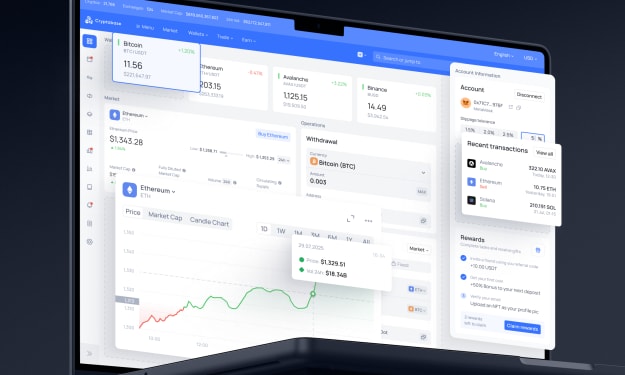
- Intelligent Search & Flexible Payments : Search should handle typos, brand/generic names, and even symptom-based queries. Filtering by form, price, or prescription status improves usability. Payments must accommodate FSA/HSA cards, insurance copays, coupons, and rebates—ideally showing real-time pricing after insurance adjudication. Use PCI-compliant gateways (e.g., Stripe) with tokenization; never store raw card data.
- Delivery Transparency : For time-sensitive meds (e.g., insulin), real-time tracking is non-negotiable. Notify users at key milestones—packed, dispatched, in transit—not with spammy alerts, but meaningful updates. Offer instant rescheduling if a delivery fails, without requiring a phone call.
Development Approach: From Concept to Launch
Discovery & Research
Start by understanding real user pain points: talk to pharmacists overwhelmed by refill calls, patients frustrated by delays, or clinic staff buried in paperwork. Analyze competitors—where do they fall short? (Maybe no one explains why a prescription was denied.) Also, clarify regulatory needs early: e-prescribing requires Surescripts; controlled substances demand DEA-compliant audit trails.
Scope Definition
Focus on your core user journey: login → view prescriptions → refill → pay → track. Nail this before adding AI or blockchain. Use prioritization frameworks (e.g., MoSCoW) to avoid feature creep. Your MVP should be the smallest version that still delights users.
UX/UI Design
Clarity and accessibility are critical. A misread dosage due to poor design could be dangerous. Ensure high contrast, screen reader compatibility, voice navigation, and resizable text. Test wireframes with real users—especially older adults—and refine based on where they struggle.
Agile Development & Rigorous QA
Work in 2–3 week sprints with regular demos. Break work into small, testable tasks. Enforce CI/CD, version control, and automated testing. QA must verify: end-to-end encryption, compliance with HIPAA/GDPR, complete audit logging, and graceful handling of edge cases (e.g., expired scripts, insurance denials). Supplement automation with manual testing—especially for usability and messaging accuracy. Conduct penetration tests and dependency scans.
Launch & Ongoing Support
Start with a pilot—e.g., one pharmacy or clinic—and gather feedback. Roll out gradually. Provide multiple support channels: in-app chat, help center, phone. Users will encounter issues; make resolution easy.
What Influences Development Costs?
Two seemingly similar apps can have vastly different price tags due to:
- Feature Scope: Basic refill + delivery vs. telehealth + EHR sync + AI = big cost difference.
- Compliance Depth: True HIPAA compliance (not just “HIPAA-ready”) requires BAAs, encryption key management, audit trails, and security testing—each adding cost. FDA or DSCSA compliance in pharma adds further layers.
- Design Quality: Accessibility, usability testing, and custom UIs cost more than templates—but are essential.
- Integrations: Connecting to Epic, Cerner, or Surescripts involves complex, time-consuming API work.
- Team Expertise: Seasoned healthcare developers cost more—but prevent costly rework from security flaws or compliance failures.
- Maintenance: Budget 15–20% of initial cost annually for updates, patches, and compliance refreshes.
Navigating Healthcare Regulations
Compliance isn’t optional—it’s foundational.
HIPAA governs how Protected Health Information (PHI) is stored, accessed, and transmitted. You’re responsible—even if using AWS or Azure.
GDPR applies if you handle any EU resident data, with stricter consent and erasure rules.
HITECH strengthens HIPAA with mandatory breach notifications and incentives for EHR adoption.
DSCSA mandates serialized, trackable drug packages across the U.S. supply chain—critical for pharma logistics software.
Future Trends Shaping the Industry
- Digital-First Care: Chronic disease management, mental health, and post-surgery recovery are increasingly remote—enabled by apps and wearables.
- True Interoperability: FHIR APIs now let patients move records between systems without custom integrations.
- Rising Patient Expectations: Over 60% of under-45 patients would switch providers for a better digital experience.
- Value-Based Care: Clinics paid for outcomes (not visits) need software to track adherence and prevent readmissions.
- Personalized Medicine: Gene therapies and tumor-specific treatments require tight coordination between labs, hospitals, and specialty pharmacies—driving demand for integrated software.
- Digital Therapeutics (DTx): FDA-cleared apps for insomnia, ADHD, and diabetes are now covered by Medicare Advantage.
- AI in Action: From predicting sepsis to matching trial patients using real-world data, AI is moving beyond hype.
- Edge Computing in IoMT: Devices like pacemakers now process data locally for real-time responses—critical in life-threatening scenarios.
- Low-Code & Open Source: Teams use low-code tools for internal apps (e.g., validation trackers), while open-source projects like OHDSI and BioPython gain traction for their transparency and auditability.
In summary, while healthcare and pharma software development comes with high barriers, it also offers unparalleled opportunities to improve lives—responsibly, securely, and at scale. With the right approach, you don’t need to be a medical expert to build something that truly matters.
About the Creator
Shakuro
We are a web and mobile design and development agency. Making websites and apps, creating brand identities, and launching startups.





Comments
There are no comments for this story
Be the first to respond and start the conversation.